ResusNation #139

A Message From Haney
Welcome to ResusNation #139

Ancient Egyptians Invented This Procedure, Then a Renaissance Doctor Mastered It!
In 1546, Italian physician Antonio Musa Brasavola achieved an impressive medical feat, performing and meticulously documenting the first successful human tracheostomy. Faced with a patient near death from severe throat obstruction due to an abscess, Brasavola courageously chose to incise the patient's windpipe—a procedure then widely considered barbaric and almost universally fatal. His account, published in his medical commentary, boldly declared, "We made the incision with these hands on a person who was about to expire…and the patient recovered." This pivotal success, meticulously recorded by the very surgeon who performed it, offered undeniable proof that the long-theorized and feared operation could, in fact, save lives.
Brasavola's triumph was particularly remarkable given the procedure's ancient and often controversial history. While the modern world credits him with the first documented success, it's fascinating to note that the earliest known depictions of a similar airway procedure can be traced back to the ancient Egyptians, dating as far back as 3600 BCE on hieroglyphic slabs. For millennia, knowledge of surgical airway access remained largely theoretical or whispered among practitioners, with its efficacy debated and its outcome almost always dire. Brasavola's 1546 case was a crucial step in transforming this ancient concept into a viable, life-saving intervention, paving the way for future advancements in surgical airway management.
Welcome to the 139th Edition of ResusNation!
Stop Using Epi Post-Arrest!
I just had a phenomenal discussion with my team about post-ROSC (Return of Spontaneous Circulation) management. We talked about the common practice of reaching for epinephrine as the initial post-arrest pressor. However when we achieve ROSC there is profound vasoplegia and the hypotension may be better served with norepinephrine. And there's data to support it; norepinephrine is the superior choice. Epinephrine, while effective during the arrest itself, comes with a hefty baggage of post-ROSC complications, including a higher risk of re-arrest, increased metabolic complications like lactic acidosis, and a higher rate of all-cause mortality.
Norepinephrine simply functions as a better pure vasopressor, by contracting those dilated arteries and veins, stabilizing hemodynamics, and reducing the damaging downstream effects of catecholamine-induced metabolic stress that we see with epinephrine. So the next time you achieve ROSC and your patient is hypotensive, consider norepinephrine as your first-line vasopressor.
Watch the full video here and leave a comment.
Don't forget to like and follow my IG, TikTok, YT, Facebook or Linkedin accounts.


Do Cardiac Patients Need More Blood After Major Surgery?
When a patient with cardiovascular disease or stroke undergoes major surgery, blood loss and the resulting anemia (low hemoglobin) are a concern. Current guidelines usually recommend a restrictive approach, where doctors only order a blood transfusion if the patient's hemoglobin level drops below 7 g/dL to conserve the blood supply and avoid potential transfusion risks. Many clinicians have questioned whether this standard is truly safe for patients at highest risk of heart complications who depend on strong oxygen delivery to vital organs. The TOP Trial, a large study involving more than 1,400 veterans who underwent large operations such as vascular surgery, was designed to answer that question. The main finding was reassuring: the liberal strategy (transfusing when hemoglobin was less than 10 g/dL) did not reduce the risk of the primary composite outcome of death or major ischemic events, including heart attack and stroke, compared to the restrictive strategy.
There was one important twist. While the restrictive approach was safe for the most critical endpoint, researchers uncovered a significant difference in other complications. Patients in the restrictive group had a higher rate of non-fatal cardiac issues at 9.9 percent, specifically new or worsening heart failure and dangerous arrhythmias, compared to 5.9 percent in the liberal group. This suggests that pushing the limits of anemia may place excess strain on an already vulnerable heart by forcing it to work harder when oxygen levels are low. Clinically, this confirms that the restrictive threshold is acceptable for preventing major events, yet it raises a caution that a slightly higher transfusion threshold may be beneficial for preventing more common but still serious cardiac complications. Doctors may need to re-evaluate transfusion triggers to better protect high-risk patients recovering from major surgery.
Here's my Takeaways:
-
Finding: The primary composite outcome at 90 days was similar between the liberal (9.1 percent) and restrictive (10.1 percent) transfusion groups. The restrictive group had a significantly higher rate of non-myocardial infarction cardiac complications at 9.9 percent versus 5.9 percent.
-
Practice Impact: The standard restrictive strategy of transfusing at hemoglobin less than 7 g/dL is safe for preventing major events and death in high-risk patients. The increased rate of heart failure and arrhythmias in the restrictive group suggests the liberal strategy of transfusing at hemoglobin less than 10 g/dL may help prevent non-fatal cardiac complications.
-
Population: Adult veterans at high risk for cardiac events, including those with histories of heart disease, stroke, or peripheral artery disease, undergoing major vascular or general surgery. Most participants were male.
-
Limitation: The primary event rate was lower than expected, reducing the power to detect differences in the main outcome. The predominantly male veteran population limits generalizability to women.
Want to learn more? Read the full study "Liberal or Restrictive Postoperative Transfusion in Patients at High Cardiac Risk: The TOP Randomized Clinical Trial" by Panos Kougias et al. in JAMA.

What’s up, ICU nerds?
Welcome! Grab a coffee and your thinking caps — let’s round.
When I say, “target MAP 80–85 mmHg in older patients with septic shock,” you’re probably thinking: “Higher = better perfusion,” right? But OPTPRESS suggests the opposite — higher may be harmful. Let’s dive in.
The Why:
-
Older adults with septic shock still carry high mortality.
-
MAP targets remain debated.
-
Chronic HTN + impaired autoregulation makes higher MAP tempting.
-
But higher vasopressor doses = possible harm.
The What:
OPTPRESS — multicenter, pragmatic, open-label RCT.
The Who:
-
518 patients ≥ 65 yrs with septic shock (Japan)
-
258 high-MAP vs 260 standard
-
~67% with chronic HTN
What’s The Intervention:
MAP 80–85 mmHg for up to 72h.
What’s The Control:
MAP 65–70 mmHg.
The Question:
Does higher MAP improve 90-day mortality?
Their Outcome:
Primary = 90-day mortality.
Secondary = support-free days, adverse events.
Let’s Talk Results:
-
High MAP target: 39.3% mortality
-
Standard: 28.6% mortality
-
Risk difference: +10.7% (95% CI 2.6–18.9)
-
Fewer RRT-free days in high-target group (which is a bad thing…)
-
No subgroup benefit — even with chronic HTN
-
Trial stopped early for harm signal
TLDR: the high MAP target group had worse outcomes.
Does this change my practice?
Not really — it just reinforces it.
-
65 Trial: lower MAP (~60–65) is safe in older vasodilatory shock.
-
OPTPRESS: higher MAP (80–85) may be harmful in older septic shock.
-
Bottom line: more pressor ≠ better perfusion, especially in stiff, older vasculature.
So I’ll keep:
→ targeting ~65–70 mmHg
→ avoiding “higher MAP just because HTN”
→ individualizing based on perfusion, not the number
This trial doesn’t shift my approach — it strengthens the case against high MAP targets in older adults.
What do you think? Game-changer — or just another data point in a messy area? Reply and let me know.
Until next time,
ICUBOY
@icuboy_meded (IG/TikTok/X/Threads)
@icuboymeded (FB)
Attention ResusNation Members...Watch the November's Videos Now!
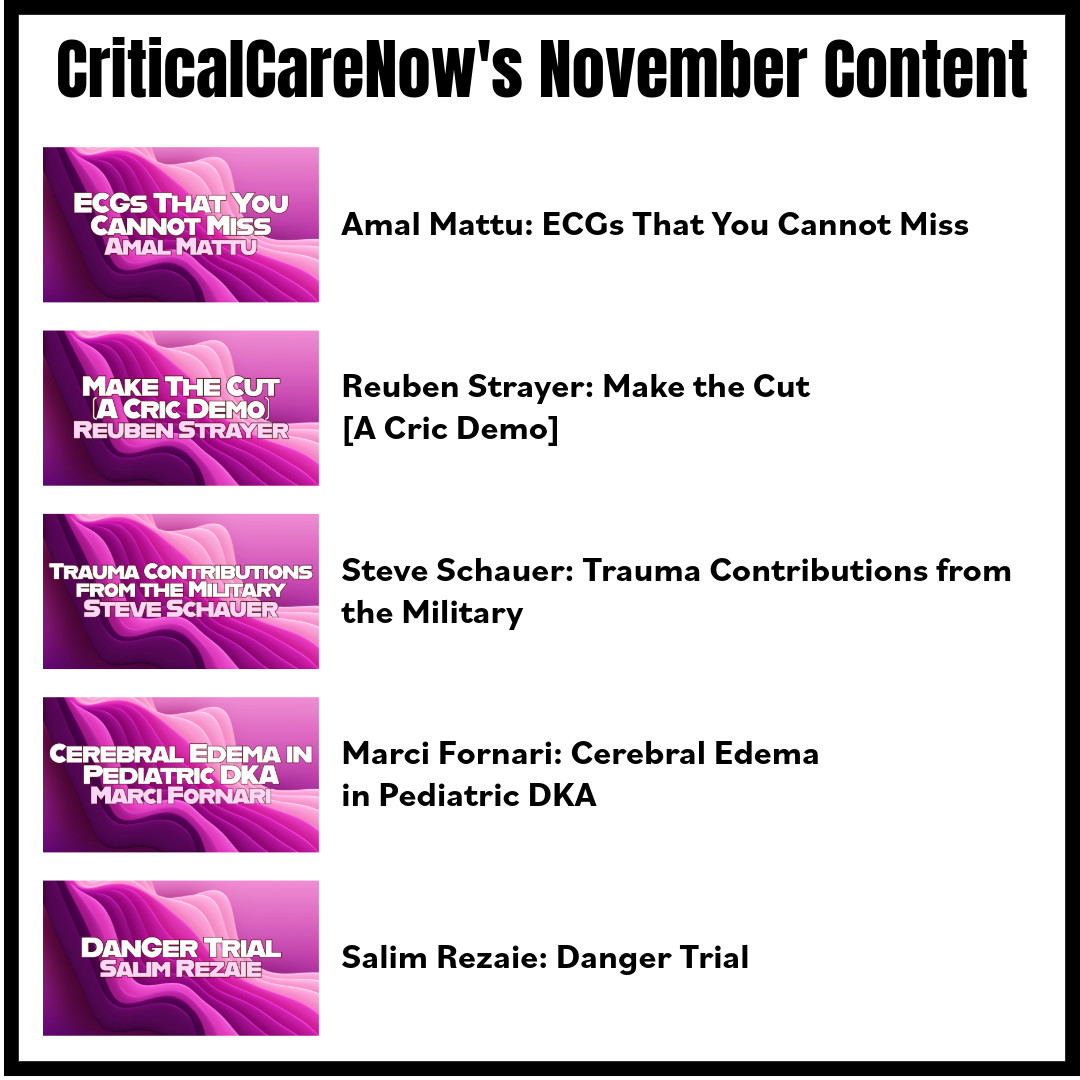
If you're an All-Access Member, you're in for some great content this month. We have FIVE videos hand-picked by our staff that are high-yield and our most highly watched. We're featuring
- Mattu on "ECGs That You Cannot Miss"
- Strayer on "Make the Cut [A Cric Demo]"
- Schauer on "Trauma Contributions from the Military"
- Fornari on "Cerebral Edema in Pediatric DKA"
- Rezaie on "Danger Trial"
Each month we bring you fresh new content from the best of the best in resuscitation. If you're an All-Access member, go watch these videos NOW! If you're not, then sign up here.


Are you a member of ResusNation? For less than a cup of coffee, you can get even more content from CriticalCareNow. Digital teaching sessions, podcasts, free video lectures, grand rounds, and so much more can be your today. Come watch on replay all the content that CriticalCareNow does live. Check out the membership options below and decide the right one for you.
Do you want even more resus content anytime you want? For less than a cup of coffee, you can get even more content from @CriticalCareNow. Digital teaching sessions, free video lectures, grand rounds, and so much more can be your today. Come watch on replay all the content that @CriticalCareNow does live.
Check out the membership options below and decide the right one for you.


Get Access To The ResusNation Today!






Responses