ResusNation #137

A Message From Haney
And They Thought It Was Just Indigestion...
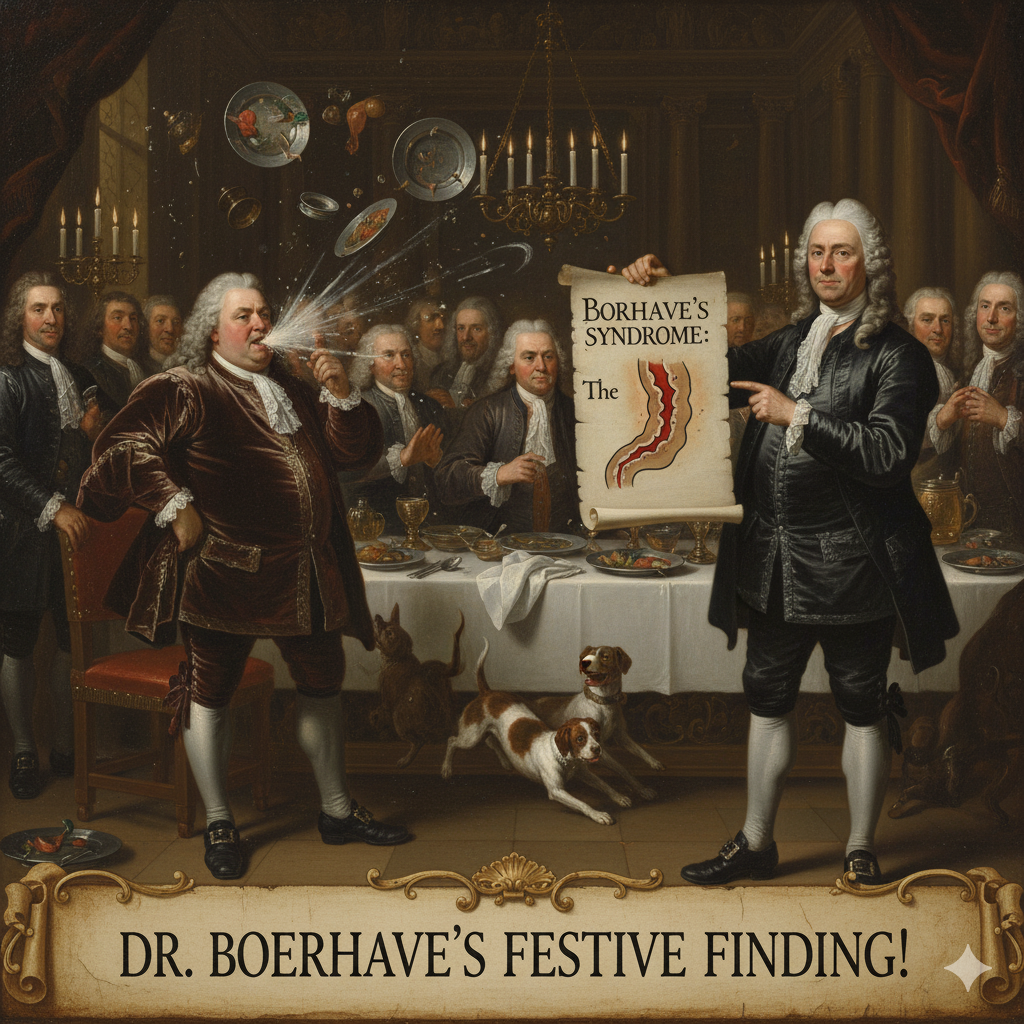
Boerhaave syndrome is a rare but critical medical condition characterized by a spontaneous, full-thickness tear or rupture of the esophagus. This sudden perforation is almost always the result of a massive surge in internal pressure, typically caused by severe or forceful vomiting and retching. When the rupture occurs, acidic stomach contents can leak into the chest cavity, leading to mediastinitis and sepsis; it's a surgical emergency with a high mortality rate if not treated immediately. Classic signs, known as the Mackler triad, include vomiting, chest pain, and air trapped under the skin (subcutaneous emphysema), though these are not always present.
The syndrome is an eponym, named for the renowned Dutch physician Dr. Herman Boerhaave (1668–1738). The story dates back to 1724 when Dr. Boerhaave attended to the unfortunate case of Baron Jan Gerrit van Wassenaer, the Grand Admiral of the Dutch Fleet. Following a lavish feast, the Admiral experienced a fatal episode of explosive vomiting. Dr. Boerhaave performed an autopsy and meticulously documented the transmural tear in the Admiral's esophagus. This careful, clinical-pathological correlation established the condition in medical literature, ensuring that the physician's name would be permanently attached to this severe form of esophageal rupture.
Welcome to the 137th edition of ResusNation!
Should I Treat That AFib RVR?
When patients present with atrial fibrillation with rapid ventricular response (AFib with RVR), the critical first step is to focus not just on the rate, but on the "why." I've seen many cases where patients with chronic AFib comes in tachycardic, and it's their heart's way of compensating for an underlying issue—think sepsis, PE, or hypovolemia. Rushing to rate-control these patients with a calcium channel blocker or beta-blocker can be a huge mistak. If their blood pressure is soft and their rate is high, taking away their compensatory tachycardia can actually tank their cardiac output and make them significantly worse. My clinical mantra here is: always treat the underlying cause first. If the rate is dangerously high (>150−160 bpm) and contributing to instability, attempt to slow it, but only after shoring up their volume status and potentially giving a short-acting vasopressor to maintain perfusion, using a low dose of an agent like diltiazem because you can always give more, but you can’t take it back.
Watch the full video here and leave a comment.
Don't forget to like and follow my IG, TikTok, YT, Facebook or Linkedin accounts.


Peripheral Lines for Pressors: A Safe Short-Term Option
When a person is in shock, vasopressors must be started quickly to normalize perfusion. Traditionally, these drugs are given through a Central Venous Catheter (CVC), because there's concern that giving them through a standard, smaller Peripheral Venous Catheter (PVC) could cause extravasation and injury to tissues. However, placing a CVC is complex, takes time, and carries its own risks of infection and complications. This new, prospective multicenter study on 250 shock patients sought to find out if the common peripheral line could be a safe alternative, and the main finding is encouraging: peripheral vasopressor administration was associated with a very low rate of extravasation injury (1.2%).
The low complication rate suggests that, especially in emergency or resource-limited settings where CVC placement is difficult or delayed, starting vasopressors through a peripheral line may be a practical, life-saving option. It's a game-changer for getting critical treatment to patients faster. However, the study uncovered a crucial detail: all three extravasation injuries occurred in patients who received the medication for five days or longer. This means that while peripheral lines are a great start, they carry a greater risk for prolonged use. The researchers recommend that doctors should safely transition patients to a central line if vasopressor therapy is anticipated to last more than a few days. While the study's high mortality rate for septic shock (67.8%) highlights the overall severity of the condition in this population, it doesn't diminish the safety finding on peripheral lines for short-term use. This research provides strong evidence to support a change in practice, which could lead to quicker stabilization and improved initial care for shock patients worldwide.
Here's my Takeaways:
-
Finding: Peripheral administration of vasopressors via PVC was associated with a low extravasation rate of 1.2% (3 out of 250 patients).
-
Practice Impact: Peripheral venous catheter (PVC) use for vasopressor administration is a safe, practical alternative to CVC for short-term use in resource-limited settings.
-
Population: Circulatory shock patients (most commonly septic shock, 69.2% ) in emergency department and ICU settings where CVC insertion is limited due to resource constraints.
- Limitation: All extravasation events occurred in patients who received vasopressors for more than five days , indicating that central access should be considered when therapy is anticipated to extend beyond a few days.
Want to learn more? Read the full study "Peripheral line for vasopressor administration: Prospective multicenter observational cohort study for survival and safety" by Adane Petros et al. in PLOS One.
Watch the October's Videos Now!

If you're an All-Access Member, you're in for some great content this month. We have FIVE videos hand-picked by our staff that are high-yield and our most highly watched. We're featuring
- Willis on "It Ain’t Sepsis, It’s a (Thyroid) Storm"
- Slovis on "Epinephrine in Arrest"
- Haywood on "Ventilation in Obesity"
- Stowens on "Where Are We With The Dizziness Paradigm?"
-
Reilly on "CT Head for the Resuscitationist - What is the Approach?"
Each month we bring you fresh new content from the best of the best in resuscitation. If you're an All-Access member, go watch these videos NOW! If you're not, then sign up here.


Are you a member of ResusNation? For less than a cup of coffee, you can get even more content from CriticalCareNow. Digital teaching sessions, podcasts, free video lectures, grand rounds, and so much more can be your today. Come watch on replay all the content that CriticalCareNow does live. Check out the membership options below and decide the right one for you.
Do you want even more resus content anytime you want? For less than a cup of coffee, you can get even more content from @CriticalCareNow. Digital teaching sessions, free video lectures, grand rounds, and so much more can be your today. Come watch on replay all the content that @CriticalCareNow does live.
Check out the membership options below and decide the right one for you.


Get Access To The ResusNation Today!






Responses