ResusNation #119

The towering giraffe is a marvel of the animal kingdom, but it faces a unique physiological challenge: how to effectively pump blood from its powerful heart all the way up its incredibly long neck to its brain. To overcome gravity's pull over such a distance, a giraffe's heart is a remarkably efficient pump, generating blood pressure roughly twice that of a human's, often reaching levels around 280/180 mmHg at the heart. Although worthy of hypertension in humans, this extraordinary pressure is essential to ensure a continuous and sufficient supply of oxygen and nutrients to its brain, even when standing at its full height.
But the challenge isn't just about pumping blood up. When a giraffe lowers its head to drink, the rapid influx of blood to its brain could be catastrophic if not managed. Nature has equipped giraffes with an ingenious system of specialized valves and highly elastic blood vessels in their necks. These adaptations act like a sophisticated pressure regulation system, preventing a sudden rush of blood to the head and allowing the giraffe to safely and efficiently quench its thirst without experiencing a dangerous increase in intracranial pressure.
Welcome to the 119th edition of ResusNation!
We Talking About LeVophed
We had a little fun this week doing the baby AI trend that you see all around and we started with talking about norepinephrine. It turns out that like me, Baby Lebron is a huge fan. Watch the full video here and leave a comment.
Don't forget to like and follow my IG, TikTok, YT, Facebook or Linkedin accounts.
Workshop Registration Is Open!
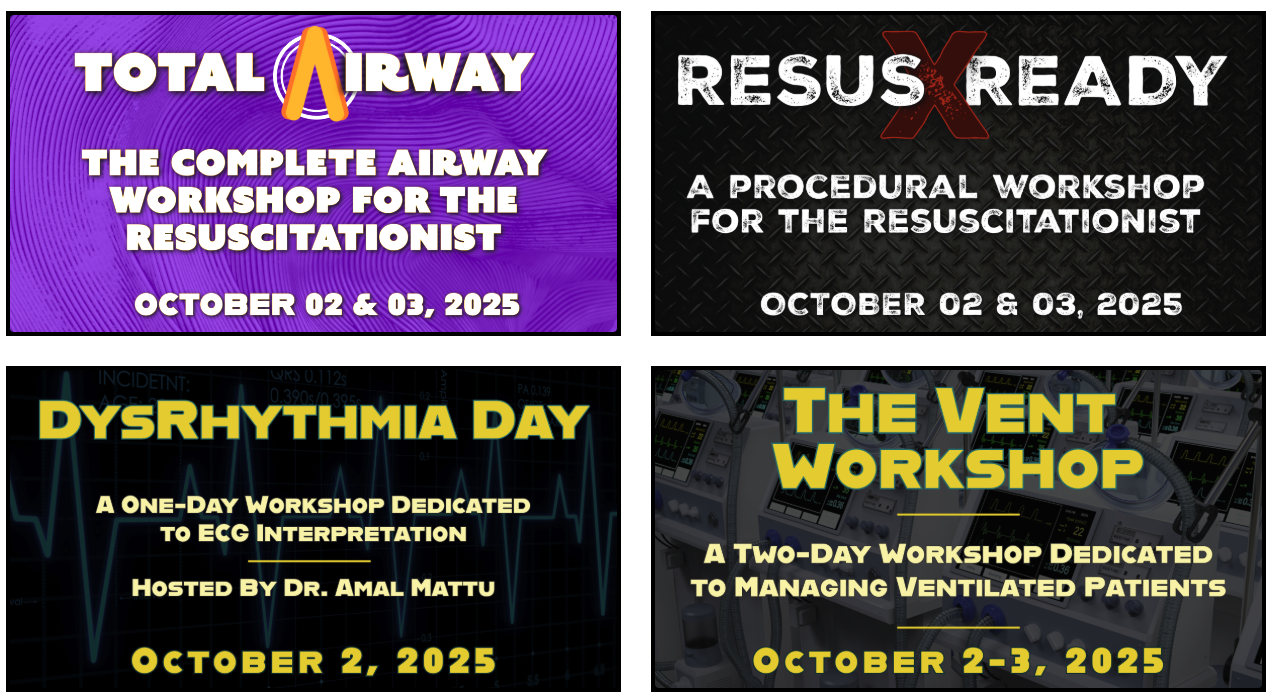
We're offering four incredible workshops in Philadelphia from October 2–3, 2025.
Led by our world-class faculty, each workshop is CME/CEU accredited and designed to meet you wherever you are in your resuscitation journey. Choose from:
-
ECG Workshop – Hosted by Dr. Amal Mattu
-
Resus Ready Workshop – A hands-on procedural workshop
-
Total Airway Workshop – Focused on intubating the sickest patients
-
The Vent Workshop – Master the art of mechanical ventilation
It's Your Call.
You can add a workshop experience to your main ResusX registration—or attend a workshop on its own without registering for the full conference.
Bonus: Register for both the conference and a workshop to unlock exclusive discounts.
GET THE RESUSX:BUNDLE (ADD-ON AT CHECKOUT)



Is Epi for Post-Arrest Shock
The Wrong Pressor?
Surviving a cardiac arrest is a monumental feat, but the battle isn't over once get ROSC. Many patients are in shock, which can lead to further complications and even another cardiac arrest. Traditionally, epinephrine has been the go-to medication to manage this shock. However, new research suggests that norepinephrine, might be a safer option, significantly reducing the chance of the heart stopping again. This is important because preventing a second cardiac arrest could greatly improve a patient's chances of a smoother recovery.
A recent review of six studies involving over 3,400 patients found that those who received norepinephrine after ROSC had a 63% lower chance of experiencing another cardiac arrest compared to those given epinephrine. While this study didn't show a clear difference in overall survival to hospital discharge or long-term brain function, the reduction in recurrent cardiac arrest is significant. Preventing re-arrest could mean less complications during recovery, even if overall survival rates weren't directly improved in this analysis. However, it's important to remember that most of the studies reviewed were observational, not controlled trials, meaning more research is needed to confirm these findings. Future studies should focus on larger, more diverse patient groups and collect more detailed information to guide doctors in choosing the best medication to support these vulnerable patients.
Here's my Takeaways:
- Finding: Patients receiving norepinephrine after return of spontaneous circulation (ROSC) had 63% lower odds of recurrent cardiac arrest compared to those receiving epinephrine.
- Practice Impact: Norepinephrine may be a better initial choice than epinephrine for managing low blood pressure after cardiac arrest, particularly for out-of-hospital cardiac arrest cases.
- Population: The study focused on adult patients (mean age 64 years, 63% male) who achieved ROSC after cardiac arrest.
- Limitation: The review included mostly observational studies and showed high variability between studies, indicating a need for more well-designed randomized controlled trials.
Want to learn more? Read the full study "Noninvasive Ventilation for Preoxygenation during Emergency Intubation" by Gibbs KW, Semler MW, Driver BE, et al. in The New England Journal of Medicine (2024).

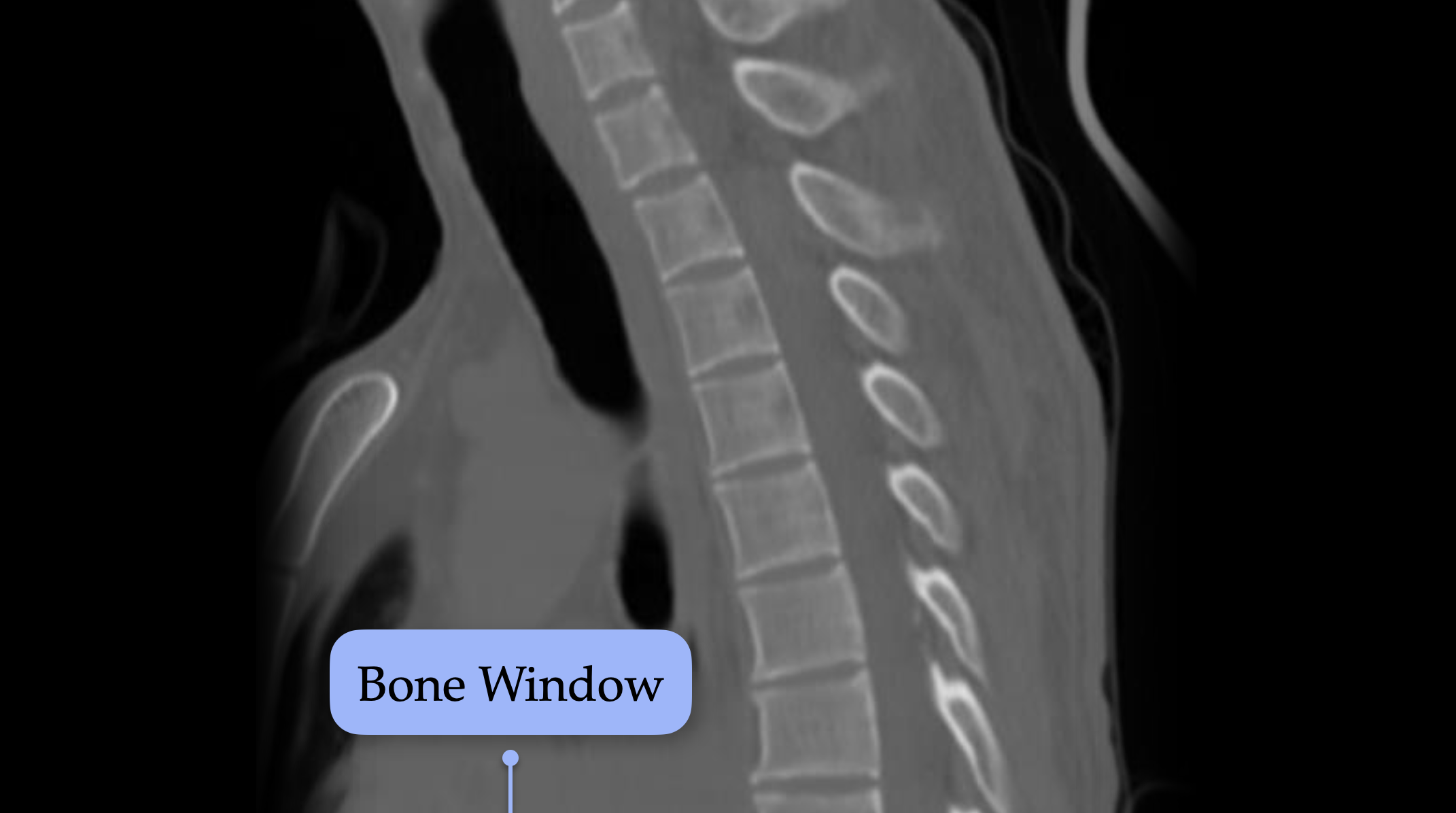
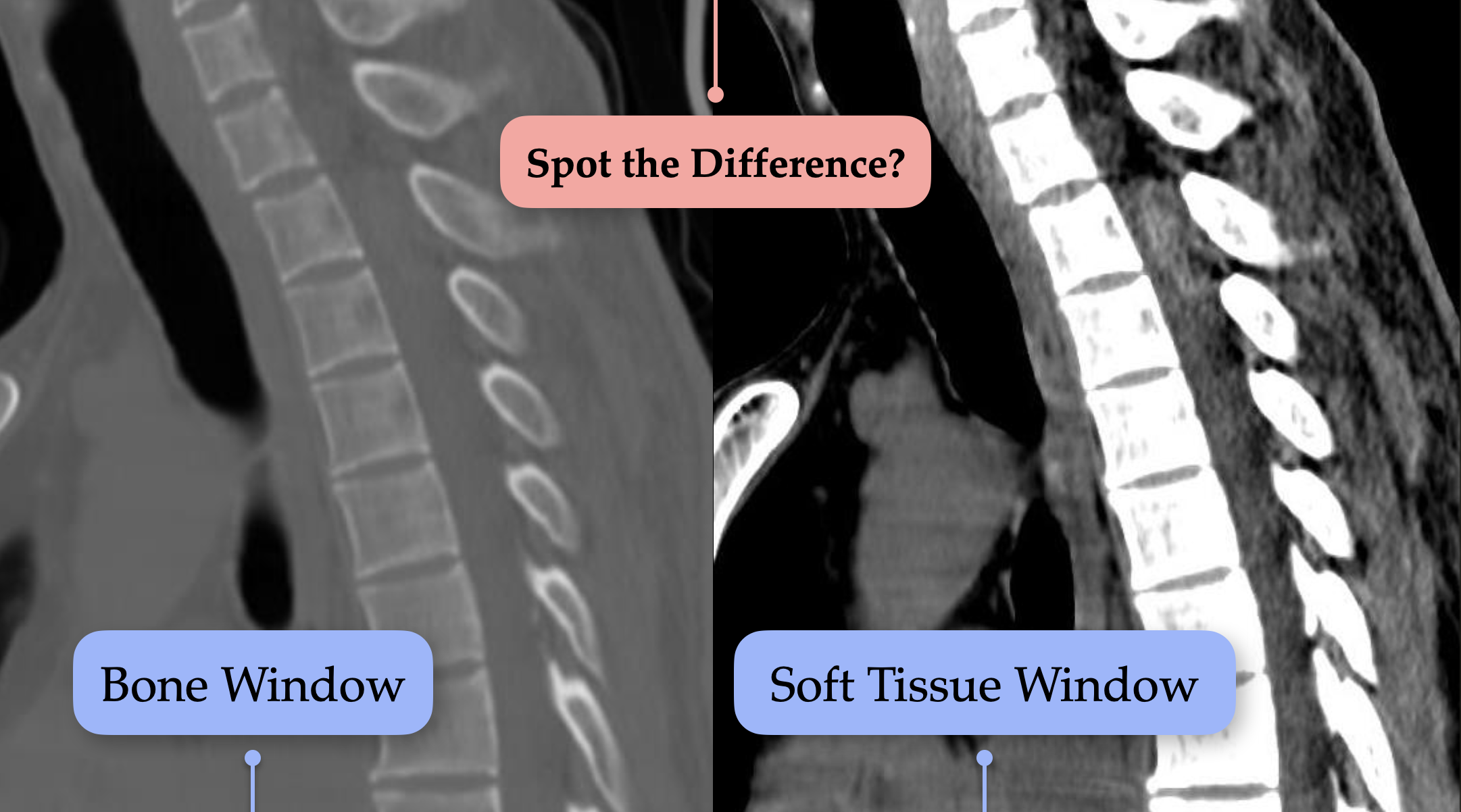
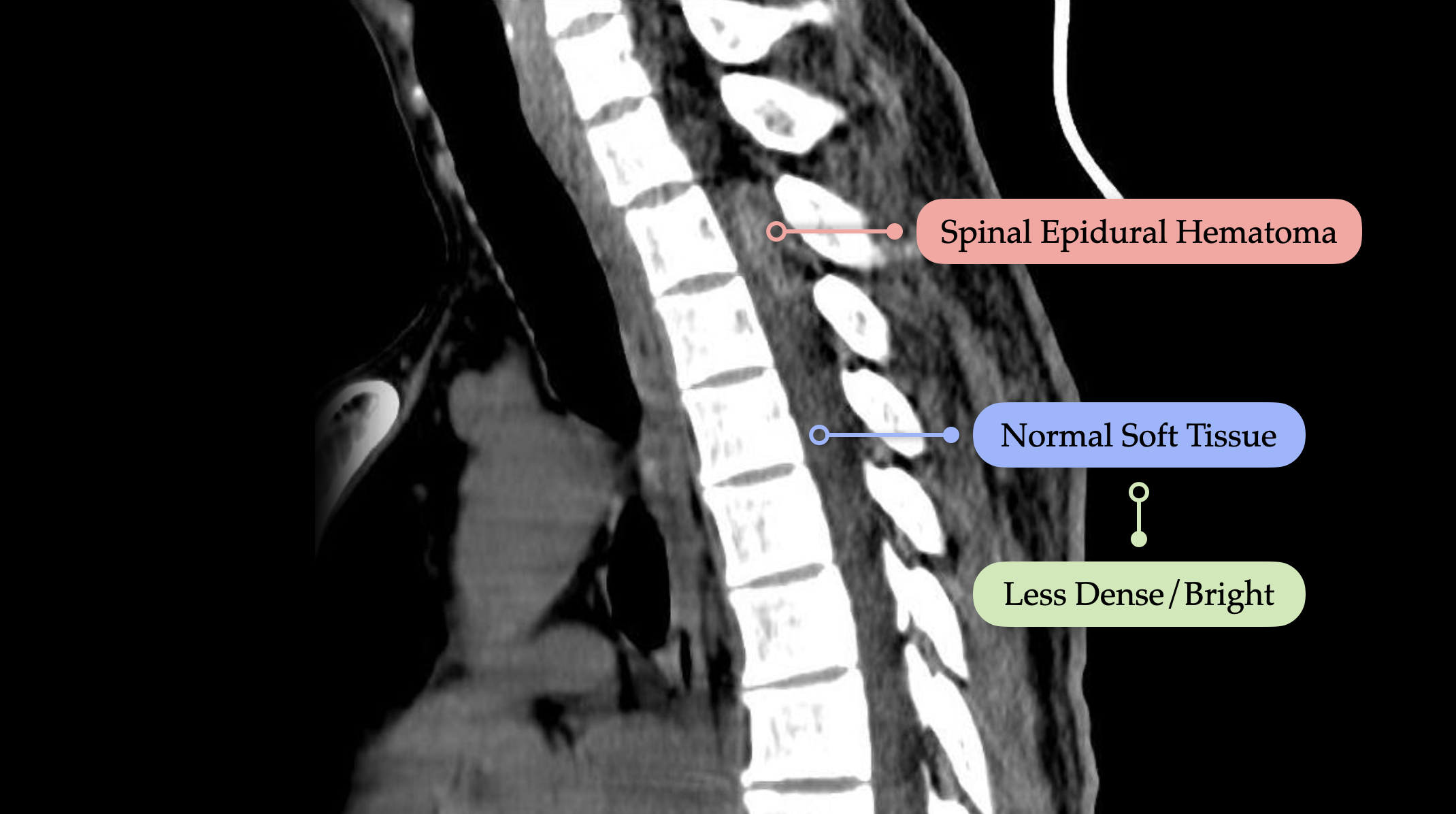
RapidRads: The right window reveals what the wrong one hides.
A patient in your department has fallen and is now reporting neck pain with paresthesias in the extremities. They have a known history of apixaban use. This is a classic setup for a spinal epidural hematoma—an easily missed but critical diagnosis.
Key takeaways:
-
Imaging of choice: Non-contrast CT of the cervical spine
-
Technique matters: Always review axial, sagittal, and coronal planes
-
Window settings: Don't rely solely on the bone window—switch to the soft tissue window to identify subtle hematomas, especially in anticoagulated patients.
Next steps:
-
Consult neurosurgery urgently
-
Consider reversal agents for anticoagulation
-
Obtain an MRI for definitive diagnosis and to assess the extent of cord compression
Watch the Rapid Diagnosis with RapidRads FULL VIDEO (quick and to the point) - courses.


Are you a member of ResusNation? For less than a cup of coffee, you can get even more content from CriticalCareNow. Digital teaching sessions, podcasts, free video lectures, grand rounds, and so much more can be your today. Come watch on replay all the content that CriticalCareNow does live. Check out the membership options below and decide the right one for you.
Do you want even more resus content anytime you want? For less than a cup of coffee, you can get even more content from @CriticalCareNow. Digital teaching sessions, free video lectures, grand rounds, and so much more can be your today. Come watch on replay all the content that @CriticalCareNow does live.
Check out the membership options below and decide the right one for you.


Get Access To The ResusNation Today!





Responses