ResusNation #134

A Message From Haney

Yet Another Benefit From Man’s Best Friend
While a dog's keen sense of smell is commonly known for tracking scents and sniffing out contraband, a growing body of research suggests that our canine companions possess an even more remarkable talent: detecting cancer. This incredible ability stems from their olfactory prowess, which is thousands of times more sensitive than a human's. Cancerous cells release unique chemical compounds, known as volatile organic compounds (VOCs), which create a distinct "odor signature" that is imperceptible to us but easily detected by a trained dog. Scientific studies have shown that dogs can accurately identify these subtle scents in various biological samples, including breath, urine, and even blood, with a high degree of accuracy.
This fascinating field of research is not about replacing traditional medical diagnostics with dogs, but rather about leveraging their unique talent to advance our understanding of cancer. By studying what exactly the dogs are smelling, scientists can identify the specific VOCs associated with different types of cancer. This knowledge is crucial for developing new, non-invasive diagnostic tools that could one day lead to earlier and more effective cancer detection. The dog's nose, a marvel of natural engineering, is providing a roadmap for a future where a simple breath test or urine sample could offer a life-saving diagnosis.
Welcome to the 134th edition of ResusNation!
End-Tidal: The REAL Way to Use It
I often hear clinicians asking if end-tidal CO2 can be a stand-in for a blood gas, and my answer is always no, at least not initially. End-tidal CO2 is influenced by ventilation, perfusion, and metabolic rate, making it an unreliable surrogate for PCO2 on its own. It's a fundamental misunderstanding of what the measurement truly represents. However, once you've established a consistent gradient with a baseline blood gas, then and only then can you use it as a surrogate for minute-to-minute changes. What I've found over my years of practice is that its real value lies in assessing physiological dead space, especially in patients with conditions like ARDS. Watching the gap between end-tidal and PCO2 narrow as you improve lung recruitment is one of the most powerful real-time indicators that your ventilatory strategy is working.
In my experience, the true utility of end-tidal CO2 isn't in a single number but in what the waveform tells you. The shape of the waveform is a direct window into patient physiology, offering clues you simply can't get from a static value. For instance, the classic "shark fin" is a dead giveaway for obstructive lung disease, signaling the need for a closer look. Similarly, a cleft in the waveform can indicate vent dyssynchrony, prompting you to reassess your settings. I even use it to differentiate between pulse oximetry lag and a true ventilation problem during a difficult intubation. This goes beyond the simple "yes/no" of tube placement and provides critical, real-time feedback that can literally save lives. It's not just a monitor; it's a dynamic diagnostic tool.
Watch the full video from Dr. Rory Spiegel here and leave a comment.
Don't forget to like and follow my IG, TikTok, YT, Facebook or Linkedin accounts.


Why Your Go-To IV Fluid Could Be Hurting TBI Patients
When a patient suffers a traumatic brain injury (TBI), every minute counts. One of the most important goals in the emergency department and intensive care unit is to maintain a healthy blood flow to the brain, preventing further damage. However, this is a delicate balance, as the wrong type or amount of fluid can worsen brain swelling and lead to a worse outcome. This recent review highlights that not all fluids are created equal, and some common practices may be causing more harm than good for TBI patients. The key takeaway is simple: maintaining stable blood pressure and fluid levels is critical, but the type of fluid used matters immensely.
The review found that for patients with TBI, the common practice of using balanced crystalloid solutions may be linked to increased mortality. A meta-analysis cited in the review found a 60% higher risk of death in patients who received balanced crystalloids compared to those who received normal saline. This is likely because balanced fluids are relatively hypotonic, meaning they have a lower concentration of salts than the blood, which can drive fluid into the injured brain tissue and worsen dangerous swelling. For this reason, European guidelines now suggest using normal saline over balanced fluids for TBI patients. The review also cautions against using albumin, another type of fluid, which has been linked to higher mortality in TBI patients. These findings suggest a need for a more personalized approach to patient care, with a clear focus on specific fluid types to avoid further complications in the most vulnerable patients.
Here's my Takeaways:
- Fluid Choice Matters: The type of fluid used for resuscitation is a critical decision in TBI management.
- Normal Saline vs. Balanced Crystalloids: Normal saline is preferred over balanced crystalloids for fluid resuscitation in TBI patients because the relative hypotonicity of balanced solutions may worsen cerebral edema. A meta-analysis found that patients who received balanced crystalloids had a 60% higher risk of death.
- Avoid Albumin: The administration of albumin in patients with TBI has been associated with significantly higher mortality compared to saline.
- Blood Pressure Targets: Hypotension, defined as a systolic blood pressure (SBP) below 90 mmHg, is linked to worse outcomes and higher mortality. Emerging research suggests that even an SBP below 110 mmHg may negatively impact mortality.
- Individualized Transfusion Strategy: There is no definitive evidence supporting either a liberal or restrictive blood transfusion strategy in TBI patients, so the approach should be tailored to individual patient's systemic and cerebral physiological parameters.
Want to learn more? Read the full study "A Comprehensive Review of Fluid Resuscitation Strategies in Traumatic Brain Injury" by Mairi Ziaka et al. in Journal of Clinical Medicine.
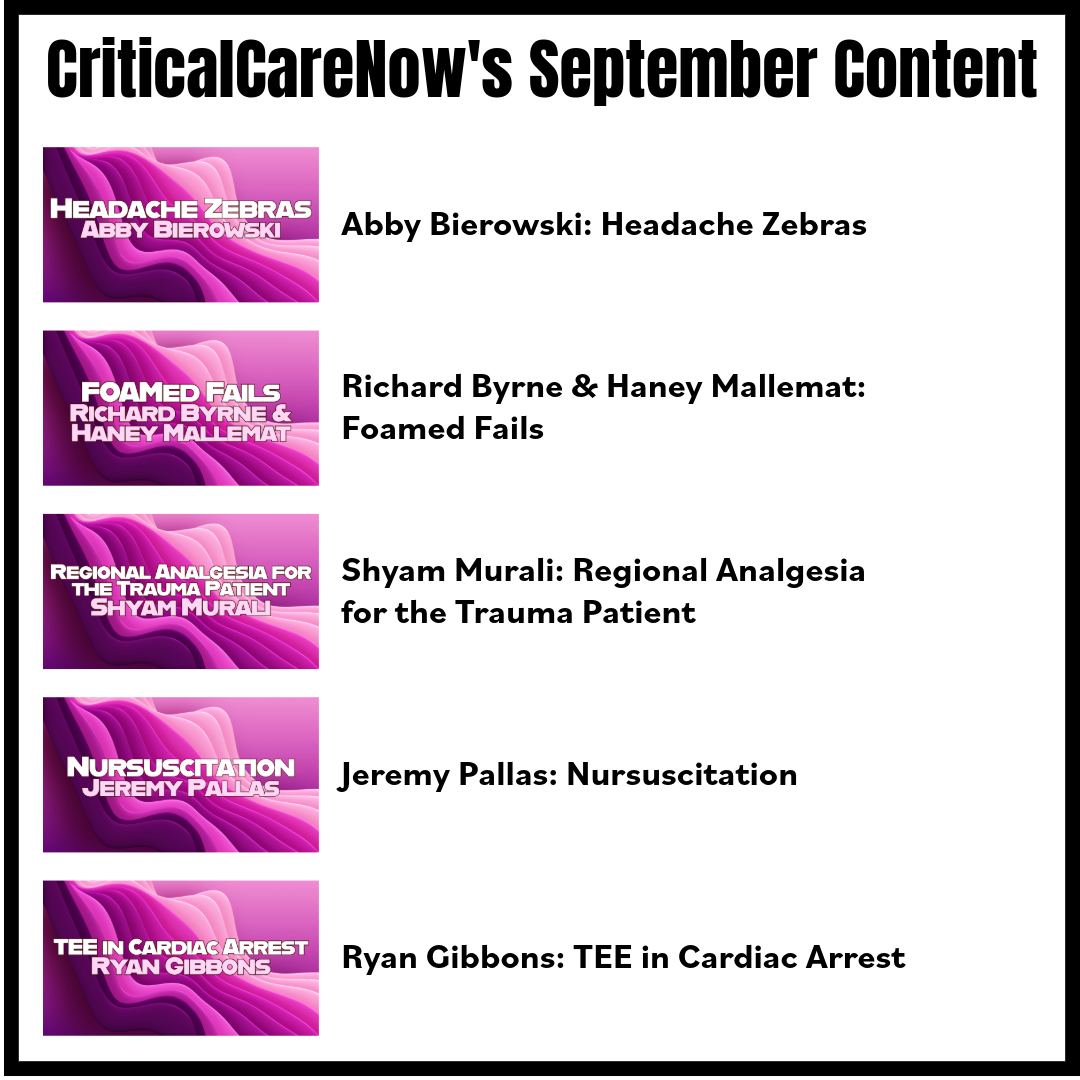
Watch the September's
Videos Now!
If you're an All-Access Member, you're in for some great content this month. We have FIVE videos hand-picked by our staff that are high-yield and our most highly watched. We're featuring
- Abby Bierowski on "Headache Zebras"
- Richard Byrne & Haney Mallemat on "Foamed Fails"
- Shyam Murali on "Regional Analgesia for the Trauma Patient"
- Jeremy Pallas on "Nursuscitation"
- Ryan Gibbons on "TEE in Cardiac Arrest"
Each month we bring you fresh new content from the best of the best in resuscitation. If you're an All-Access member, go watch these videos NOW! If you're not, then sign up here.


Are you a member of ResusNation? For less than a cup of coffee, you can get even more content from CriticalCareNow. Digital teaching sessions, podcasts, free video lectures, grand rounds, and so much more can be your today. Come watch on replay all the content that CriticalCareNow does live. Check out the membership options below and decide the right one for you.
Do you want even more resus content anytime you want? For less than a cup of coffee, you can get even more content from @CriticalCareNow. Digital teaching sessions, free video lectures, grand rounds, and so much more can be your today. Come watch on replay all the content that @CriticalCareNow does live.
Check out the membership options below and decide the right one for you.


Get Access To The ResusNation Today!





Responses