ResusNation #133

A Message From Haney

The One Pill You Take That Scientists Still Don't Get
Acetaminophen, a medication found in popular brands like Tylenol is a staple in medicine cabinets worldwide for its ability to combat pain and fever. Despite its widespread and long-standing use, some aspects of this drug remain a puzzle to scientists. Its exact mechanism of action, for instance, is not fully understood. While it's believed to inhibit an enzyme called cyclooxygenase (COX) in the central nervous system, this effect is highly selective and differs from that of NSAIDs like ibuprofen, which act more broadly throughout the body. Interestingly, the drug was discovered by chance in the late 19th century when researchers were mistakenly given a different chemical that was found to reduce fever. Additionally, it's known as "paracetamol" in most parts of the world, highlighting a fascinating difference in naming conventions.
While acetaminophen is generally considered safe when used as directed, it is not without its risks. It has a "ceiling effect," meaning that taking more than the recommended dose does not provide additional pain relief and instead significantly increases the risk of side effects, especially liver damage. This is a critical point, as acetaminophen overdose is the leading cause of acute liver failure in the Western world. Many of these overdoses are unintentional, often occurring when people unknowingly take multiple medications—such as cold and flu remedies or certain prescription pain relievers—that all contain acetaminophen. Understanding these nuances is crucial for safe and effective use of this ubiquitous medication.
Welcome to the 133rd edition of ResusNation!
Redefining Post-Arrest Care"
It's tempting to rush every post-cardiac arrest patient with a suspected cardiac cause straight to the cath lab. I've been there myself, wanting to clear the department and get the patient definitive care. But over my 20-plus years in emergency medicine, I've learned that a knee-jerk reaction isn't always the best one, especially when the patient has a return of spontaneous circulation (ROSC). The initial post-arrest EKG can be a minefield of misleading information due to the trauma of CPR, defibrillation, and administered epinephrine. I've had more than one interventional cardiologist tell me to repeat an EKG because the initial one looked suspicious, only to find the ST elevations had resolved. It feels counterintuitive to wait, but allowing that washout period is critical.
This experience-based approach is now backed by solid data. Studies like Tomahawk and COACT have shown that for patients with ROSC who do not have a clear STEMI pattern on their EKG, immediate, routine catheterization does not improve outcomes and may even increase mortality. This evidence challenges the old "send them all to the cath lab" mentality. Instead, a more deliberate, thoughtful approach is required. We must perform a thorough evaluation, rule out other causes, and use our clinical judgment. This doesn't mean we abandon the patient; it means we reserve the cath lab for those who will truly benefit—patients with a clear STEMI, ongoing cardiogenic shock, or an unstable, dysrhythmic course. We have to be smart about when we activate an entire team in the middle of the night.
Watch the full video here and leave a comment.
Don't forget to like and follow my IG, TikTok, YT, Facebook or Linkedin accounts.
20 Days Until ResusX !
ResusX:2025 is the most anticipated resuscitation conference of 2025 is almost sold-out! Come to historic Philadelphia and spend three-days watching the Rockstars of Resuscitation in action. You'll see short format, high-energy talks, interviews, procedure demoes, and debates. ResusX is not simply a conference, but a resuscitative experience where you are part of the show and spend lots of time after the conference hanging out with the faculty.
Registration will not only give you full-access to the conference but also a swag bag filled with a t-shirt, stickers, and a ton more. Food and snack is on us and you'll also be elibigble to earn up to 20.0 CME or CEU credit. We got your trip covered with on-site parking and an available hotel block.
GET SHESE BONUSES!
- Lifetime access to ResusX:2024 + CME / CEUs
- Lifetime access to ResusX:2023 + CME / CEUs
- FREE Ticket to ResusEM Live in Philly on October 9th. Attend Live or Virtually
We will also be offering a selection of post-conference workshops on October 2 & 3 including:
- Amal Mattu's ECG workshop
- UltraRounds: the resuscitative ultrasound workshop
- ResusReady: a procedural workshop for resuscitationists
Today is your opportunity to take your resuscitation skills to the next level and save big with our early-bird discounts. Come to ResusX, learn the skills and save more lives. Click on the link below to register for your early-bird tickets now.



The Clock Is Ticking: New Study Reveals Shorter ECPR Window for Elderly Cardiac Arrest Patients
When someone has a sudden cardiac arrest outside of a hospital, every second counts. For patients who don't respond to standard CPR, Extracorporeal Cardiopulmonary Resuscitation (ECPR) can be used. ECPR acts as a temporary replacement for the heart and lungs, but getting it started quickly is essential. This new research shines a light on a critical question: how long do we really have? The study found that while ECPR can save lives, the time window for it to be effective is significantly shorter for older patients, a finding that could change how emergency teams respond.
The study, which looked at data from a large number of patients in Korea, revealed a big difference between age groups. For patients 65 and younger, the chances of survival remained viable for a longer period, with a 10% survival probability holding for up to 38 minutes of ECPR initiation time. However, for elderly patients (over 65), that same probability plummeted after only 21 minutes. This finding suggests that the standard 60-minute guideline for ECPR initiation may be too late for older individuals. While the study has some limitations due to its retrospective design , the results highlight the urgent need for a faster, more targeted approach to ECPR for elderly patients. The authors recommend that teams aim to initiate the procedure within 20 minutes of a patient's arrival at the hospital for the best chance of survival.
Here's my Takeaways:
- Finding: The effective time window for starting ECPR is significantly shorter for elderly patients. Specifically, the probability of survival for elderly patients dropped below 10% if ECPR was delayed beyond 21 minutes, compared to 38 minutes for non-elderly patients.
- Practice Impact: For the best chance of survival, medical teams should make rapid decisions and initiate ECPR in elderly individuals almost immediately upon arrival, ideally within 20 minutes. This challenges the current guideline of a 60-minute window, which may be too long for this specific patient group.
- Population: The study was a nationwide observational study of 483 adult patients who received ECPR for out-of-hospital cardiac arrest in Korea. Patients were divided into two groups: those 65 years and younger and those older than 65.
- Limitation: The study was retrospective, meaning it relied on past data, which could introduce potential selection bias or a lack of detailed information on the quality of CPR. The findings may also not be generalizable to other healthcare systems.
Want to learn more? Read the full study "Impact of ECPR initiation time and age on survival in out-of-hospital cardiac arrest patients: a nationwide observational study" by Kim et al. in Critical Care.
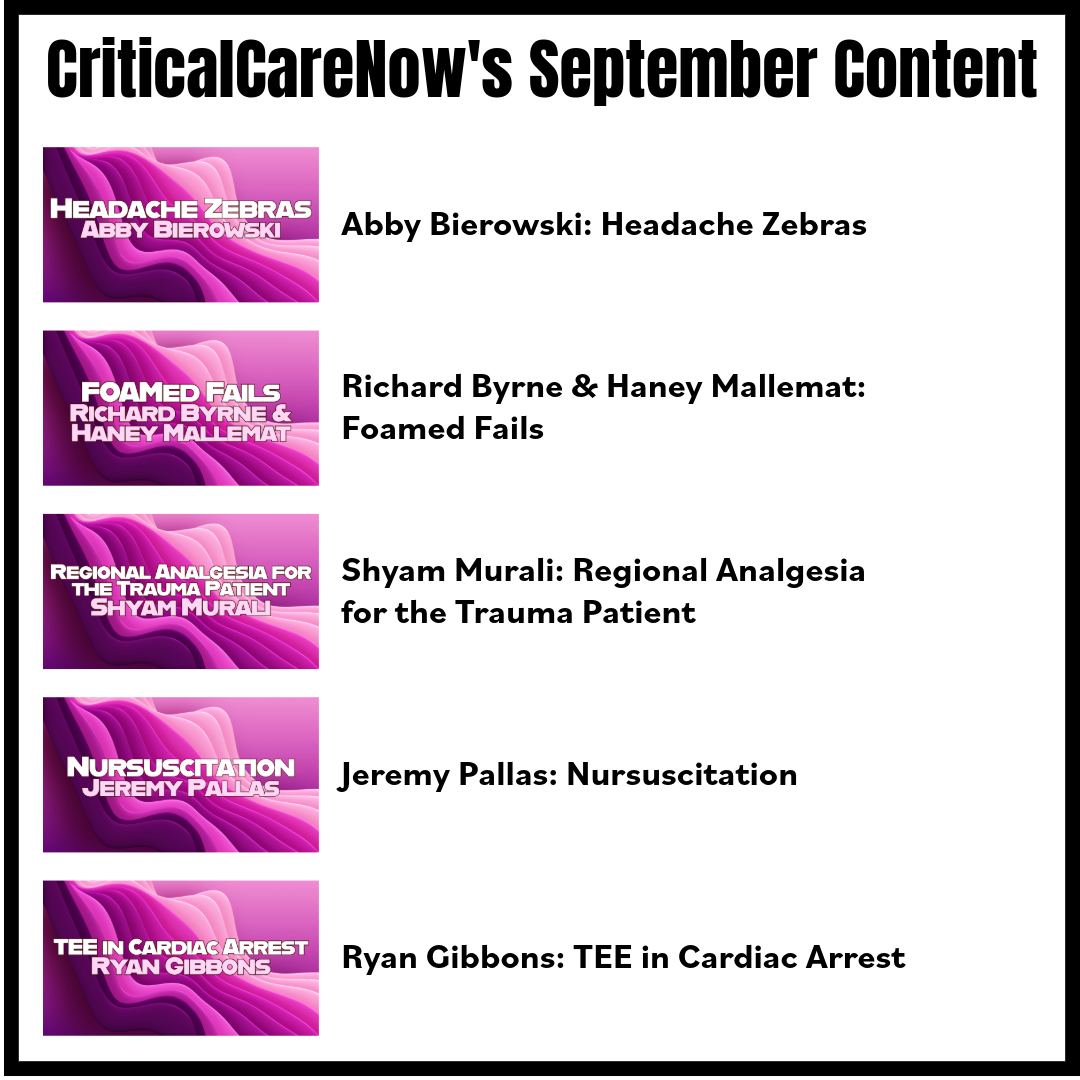
Watch the September's
Videos Now!
If you're an All-Access Member, you're in for some great content this month. We have FIVE videos hand-picked by our staff that are high-yield and our most highly watched. We're featuring
- Abby Bierowski on "Headache Zebras"
- Richard Byrne & Haney Mallemat on "Foamed Fails"
- Shyam Murali on "Regional Analgesia for the Trauma Patient"
- Jeremy Pallas on "Nursuscitation"
- Ryan Gibbons on "TEE in Cardiac Arrest"
Each month we bring you fresh new content from the best of the best in resuscitation. If you're an All-Access member, go watch these videos NOW! If you're not, then sign up here.


Are you a member of ResusNation? For less than a cup of coffee, you can get even more content from CriticalCareNow. Digital teaching sessions, podcasts, free video lectures, grand rounds, and so much more can be your today. Come watch on replay all the content that CriticalCareNow does live. Check out the membership options below and decide the right one for you.
Do you want even more resus content anytime you want? For less than a cup of coffee, you can get even more content from @CriticalCareNow. Digital teaching sessions, free video lectures, grand rounds, and so much more can be your today. Come watch on replay all the content that @CriticalCareNow does live.
Check out the membership options below and decide the right one for you.


Get Access To The ResusNation Today!






Responses