ResusNation #141

A Message From Haney
Look at the B*lls On That Guy!
Imagine a "doctor" whose solution to every man's midlife crisis wasn't a sports car, but surgically implanting goat testicles into their scrotums. Yes, you read that right. In the 1920s, John Brinkley became a millionaire by convincing thousands of men that the secret to eternal virility was a pair of "goat glands" (specifically from frisky young goats). It was a simpler time, when medical licenses were optional and the placebo effect was apparently powerful enough to make people overlook the fact that they had barnyard parts stitched under their skin.
But wait, it gets crazier! This quack didn't just stop at medical malpractice; he used his goat-gland fortune to build the world's most powerful radio station in Mexico (to dodge U.S. laws) and nearly got himself elected governor of Kansas. His empire was built entirely on radio waves and the gullibility of men desperate for a miracle. If you think today's health fads are wild, just remember: at least nobody is trying to sell you a "procedure" involving a baby goat and a scalpel. You have to read the full story of this bonkers con man to believe it
Welcome to the 141st edition of ResusNation!
Master These 3 Vent Basics First
Frankly, the current "alphabet soup" of proprietary ventilator modes gives even experienced clinicians imposter syndrome. But here’s the hard truth: while we’re obsessing over complex algorithms like PRVC or ASV, we are neglecting the fundamentals that actually drive mortality. Retrospective data shows that 40% of patients—particularly women and those of shorter stature—are still receiving inappropriately high tidal volumes (>8 mL/kg). We are damaging lungs because we’re "eyeballing" patient height rather than using a tape measure to calculate predicted body weight.
The same negligence applies to oxygenation. We need to break the reflex of blindly starting every intubated patient on 100% FiO2. The "safe landing zone" for PaO2 is between 75 and 120 mmHg; once you cross 200 mmHg, survival rates plummet due to hyperoxic injury. Before you worry about advanced closed-loop systems, ensure you are nailing the life-saving basics: strict low tidal volume ventilation, aggressive avoidance of hyperoxia, and proning for severe ARDS (P/F ratio <150). Master the fundamentals first; they are the only settings guaranteed to save your patient.
Watch the full video here and leave a comment.
Don't forget to like and follow my IG, TikTok, YT, Facebook or Linkedin accounts.
Missed the Black Friday Sale?
No Worries — I’ve Got You.
It’s the season of giving, and I’m opening up something special. As a thank-you for being part of the ResusX community, I’m giving you FREE access to our brand-new ResusX:2025 Mini Course — packed with four high-yield, full-length talks from some of the biggest names in resuscitation.
Here’s what you’re getting for free:
-
Trauma Airway Logic with Dr. Carunchio
-
Widow-Maker ECGs with Dr. Mattu
-
Airway Strategy with Dr. Strayer
-
ECMO Physiology with Dr. Crager
This is your holiday gift from us: real education, zero cost, and a front-row seat to the level of learning you’ll experience at ResusX:2025.
Tap in and start the Mini Course now.
Strengthen your skills. Sharpen your instincts. Elevate your practice.



Combined NIV and High-Flow Oxygen Shows No Benefit
When patients arrive at the hospital struggling to breathe, the team’s first instinct is often to throw every available tool at the problem to keep them off a mechanical ventilator. It seems logical that combining two powerful support methods—a pressurized face mask (NIV) and high-flow heated oxygen (HFNC)—would work better than using just one alone. However, a new analysis of over 700 patients challenges this "more is better" assumption. Researchers found that using both therapies together as the first-line treatment did not actually reduce the need for intubation compared to using either method by itself.
This finding is a big deal for hospitals because it suggests that adding complexity to patient care doesn't always lead to better results. The data showed no survival benefit to the combined approach, meaning patients did just as well with simpler, single-mode therapy. While the study noted that the success of mask ventilation might depend on using gentle settings to protect the lungs, the overall message is clear: doubling up on equipment didn't save more lives. For now, clinicians can feel confident sticking to established, simpler protocols, sparing patients the potential discomfort of a complex setup unless future research proves otherwise.
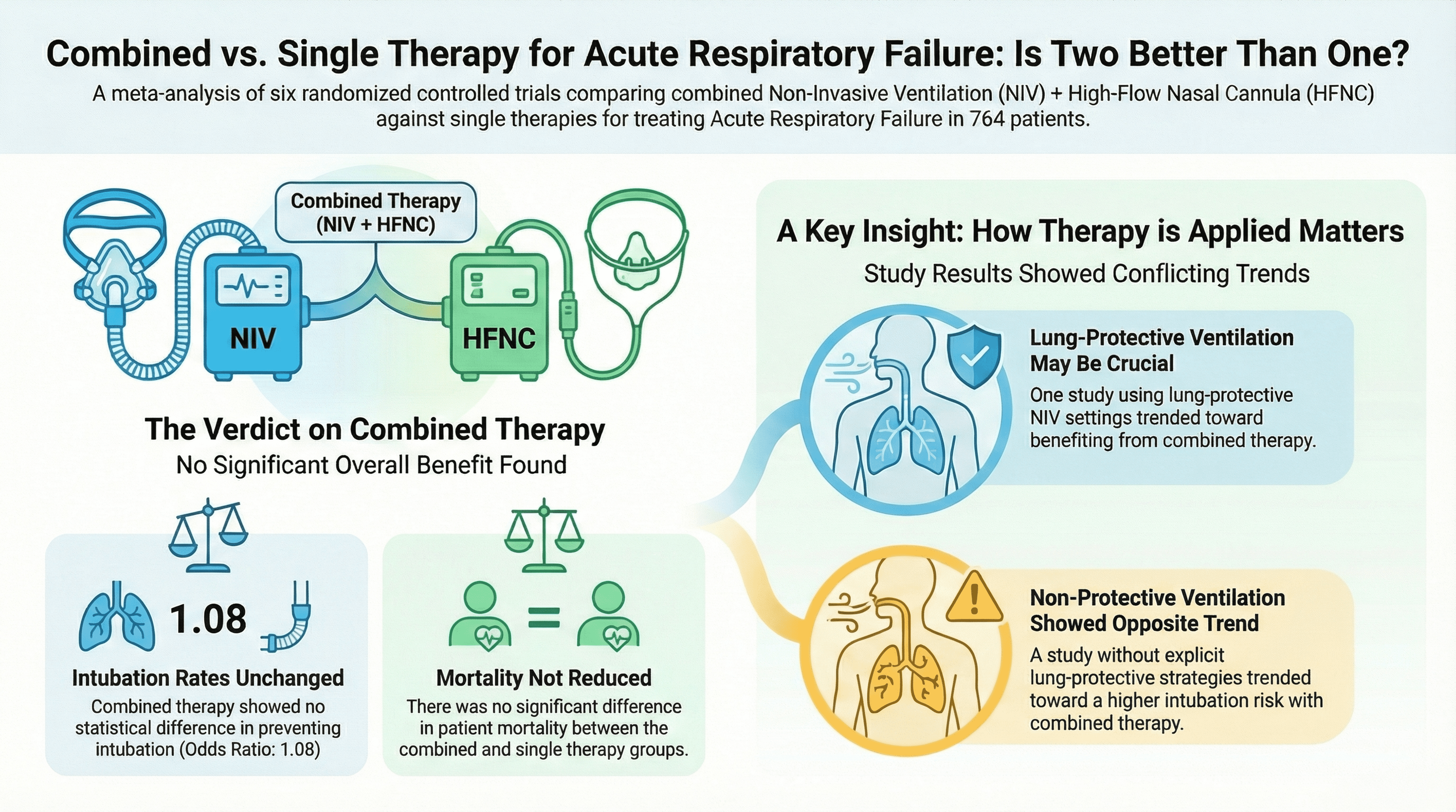
Here's my Takeaways:
- Finding: Initial treatment with combined NIV and HFNC did not significantly reduce intubation rates (OR 1.08) or mortality (OR 1.41) compared to monotherapy.
- Practice Impact: Routine combination of these devices for initial acute respiratory failure treatment is not recommended; clinicians should stick to standard single-device therapy to avoid unnecessary complexity.
- Population: 764 adults with acute respiratory failure (ARF) across 6 randomized controlled trials (RCTs).
- Limitation: The included studies had a high risk of performance bias (unblinded), and inconsistent use of lung-protective ventilation strategies may have skewed results.
Want to learn more? Read the full study "Efficacy of HFNC + NIV as initial oxygen therapy in acute respiratory failure: Meta-analysisere" by Weizhong Wang et al. in the American Journal of Emergency Medicine.
Bicarbonate is not a reflex; it is a precision therapy. Despite its frequent use for "low numbers" on a blood gas, sodium bicarbonate is often ineffective or even harmful when used indiscriminately for pure lactic acidosis, sepsis without AKI, or respiratory acidosis. A major pitfall highlighted is the use of "push-dose" hypertonic bicarbonate in hyperkalemic arrests; this can paradoxically worsen serum potassium levels due to "solute drag," where the rapid osmotic shift pulls potassium out of cells. Furthermore, rapid CO₂ generation from boluses can worsen intracellular acidosis and depress myocardial contractility, arguing against its routine use as a universal antidote for acidemia.
Evidence supports targeted use in specific phenotypes. The strongest data (BICAR-ICU trials) supports bicarbonate use for severe metabolic acidemia (pH ≤ 7.2) associated with Acute Kidney Injury (AKI), where it may reduce the need for renal replacement therapy. For resuscitation requiring both volume and alkali, the author recommends isotonic bicarbonate (150 mEq NaHCO₃ in 1L D5W) over hypertonic boluses to avoid sodium load and hypertonicity risks. Ultimately, clinicians should move from "treating the number" to a pH-guided resuscitation strategy that reserves bicarbonate for cases where acidemia is truly maladaptive, such as severe AKI, hyperchloremic acidosis, or specific toxicities like TCA poisoning.
Please read my full post here
Watch the December's
Videos Now!
If you're an All-Access Member, you're in for some great content this month. We have FIVE videos hand-picked by our staff that are high-yield and our most highly watched. We're featuring
- Spiegel on "65% of the Time The Bougie Works Every Time"
- Khoujah on "Status Epilepticus"
- Crager on "Should That Patient Be On ECMO?"
- Willis on "This Ain't Your Daddy's DKA"
- Byrne on "The Trauma Airway"
Each month we bring you fresh new content from the best of the best in resuscitation. If you're an All-Access member, go watch these videos NOW! If you're not, then sign up here.






Responses