ResusNation #143


Human GLP-1 is Weak. Lizard Venom is Forever.
Look, Endocrinology is mostly just trying to gaslight the pancreas into doing its job properly. For years, we struggled because human GLP-1 is incredibly fragile; it has a half-life of less than two minutes because the enzyme DPP-4 chews it up faster than a resident inhaling a granola bar between cases. Enter the Gila monster (Heloderma suspectum), a venomous lizard from the American Southwest that spends 95% of its life underground avoiding social interaction (relatable). Researchers discovered that when this lizard actually bothers to eat, its toxic saliva contains a peptide called Exendin-4, which is essentially GLP-1 on steroids.
Here is the kicker: unlike our pathetic human version, the Gila monster’s peptide is structurally resistant to DPP-4 degradation. It enters the bloodstream, completely ignores the enzymes trying to kill it, and screams at the beta cells to release insulin until glucose levels normalize. It is the biological equivalent of a tank. So, naturally, we decided to synthesize this venom, put it in a pen, and call it Exenatide (Byetta). We are essentially treating Type 2 Diabetes by borrowing the evolutionary superpowers of a spicy desert reptile, proving once again that nature is both terrifying and helpful.
Welcome to the 143rd edition of ResusNation!
Don't Sleep on the IO
Let’s be honest about what actually constitutes a "crash line" versus bad practice. If you have the time to grab an ultrasound, set up a probe cover, and prep the machine, you are no longer in "crash" territory—you are placing a sterile line. If you do all that heavy lifting but skip the drape or full sterile barrier, I’m going to say something controversial: that isn’t urgency, that is just laziness. True crash lines have their place when a patient is actively dying, but we need to stop using the term as an excuse for cutting corners on patients who are stable enough for proper technique.
Furthermore, if the patient is truly crashing, why are we still fighting for femoral or subclavian access in 2026? We are completely sleeping on the Intraosseous (IO) line. It is arguably the most underutilized tool in modern resuscitation. You can infuse absolutely anything through an IO that you can through a central line. Instead of wasting critical minutes struggling with a difficult stick during a code, grab the drill. It’s time to stop letting ego dictate our access points and start prioritizing speed and efficacy.
Watch the full video here and leave a comment.
Don't forget to like and follow my IG, TikTok, YT, Facebook or Linkedin accounts.


Is Normal Saline Actually Better for Brain Injury Patients?
For years, emergency medicine providers have debated the best fluids to use when reviving trauma patients, with a recent trend favoring "balanced" fluids over traditional normal saline. However, a new systematic review is challenging that shift, suggesting that the "old school" option might actually save more lives in specific cases. The study analyzed data from nearly 2,000 patients and discovered a critical difference: for patients with Traumatic Brain Injury (TBI), those treated with normal saline had significantly lower death rates and spent fewer days on ventilators compared to those treated with balanced fluids. This difference likely comes down to sodium levels; normal saline has a higher sodium concentration, which can help prevent dangerous brain swelling (cerebral edema) that balanced fluids might inadvertently worsen. Importantly, for trauma patients without brain injuries, the study found no difference between the fluids regarding survival or kidney safety, meaning balanced fluids are still safe for general injuries. However, because it is often impossible to rule out head trauma in the chaotic first minutes of resuscitation, the authors conclude that sticking with normal saline remains a widely safe and standardized strategy for early trauma care.
Here's my Takeaways:
- Finding: Normal saline was associated with significantly lower mortality (OR 1.35) and more ventilator-free days compared to balanced crystalloids in patients with traumatic brain injury (TBI), while no significant difference was found in trauma patients without
- Practice Impact: Since it is often impossible to rule out head injury during initial resuscitation, normal saline remains the safest standardized fluid option for undifferentiated trauma patients to avoid worsening cerebral edema
- Population: 1,950 trauma patients requiring fluid resuscitation, stratified by those with and without traumatic brain injury across six randomized controlled trials
- Limitation: The review relied exclusively on randomized controlled trials, which may limit generalizability to real-world settings, and inconsistent reporting of injury severity prevented detailed subgroup analysis based on trauma severity
Want to learn more? Read the full study "Balanced crystalloids versus normal saline for trauma resuscitation: A systematic review and meta-analysis" by Zaki et al. in the American Journal of Emergency Medicine.

ResusX:2026 Is Here — Register Now!
Save the Date: May 18–20, 2026
We’re thrilled to officially announce that ResusX:2026 is happening — and it’s coming back bigger, bolder, and more immersive than ever.
Now entering its eighth year, ResusX returns May 18–20, 2026, once again taking over Philadelphia’s iconic Punch Line Comedy Club for three days of high-impact resuscitation education, community, and connection.
The excitement from ResusNation has been incredible, and we’re ready to make this our most anticipated event yet. Expect an unforgettable experience with:
-
Leading voices in resuscitation
-
Cutting-edge clinical discussions
-
Energy and community that make ResusX unlike any other conference

We’re also finalizing:
-
A dynamic, action-packed conference schedule
-
Specialized post-conference workshops
-
Full CME and CEU details (coming soon)
With an intimate venue and consistently strong demand, ResusX has a history of selling out — and 2026 is no exception.
📍 Philadelphia, PA
📅 May 18–20, 2026
🎤 Punch Line Comedy Club
🔥 Spots are open now — secure your place today!
More details coming soon, but don’t wait — ResusX:2026 is on the way, and seats will go fast.
The A.D.D. Approach to Becoming More Productive
Intubating patients with severe metabolic acidosis poses a critical risk of hemodynamic collapse due to the abrupt loss of compensatory respiratory alkalosis. Once sedated and paralyzed, the patient's intrinsic drive to hyperventilate is eliminated, potentially leading to a rapid rise in PaCO2 and worsening acidemia. The primary goal of mechanical ventilation in these cases is not to normalize pH immediately, but to bridge the gap by replicating the patient's pre-intubation compensatory minute ventilation. This strategy aims to maintain a safe pH (generally ≥ 7.15) while treating the underlying cause, avoiding the common pitfall of standard ventilator settings that fail to meet the patient's extreme physiologic demand.
To achieve this safely, Volume-Controlled Ventilation (VCV) is recommended because it guarantees a predictable minute ventilation. The strategy involves setting a high respiratory rate (often 24–35 breaths/min) as the primary lever, combined with a tidal volume of 6–8 mL/kg predicted body weight (or strictly 6 mL/kg if lung injury is present). Clinicians should estimate the required PaCO2 using Winter’s equation and consider "pre-ventilation"—maintaining high minute ventilation during the apneic period—for high-risk cases like DKA. Continuous monitoring of EtCO2 trends and serial ABGs is non-negotiable to ensure the ventilator is effectively doing the work the patient can no longer sustain.
Please read my full post here
Watch the January's
Videos Now!
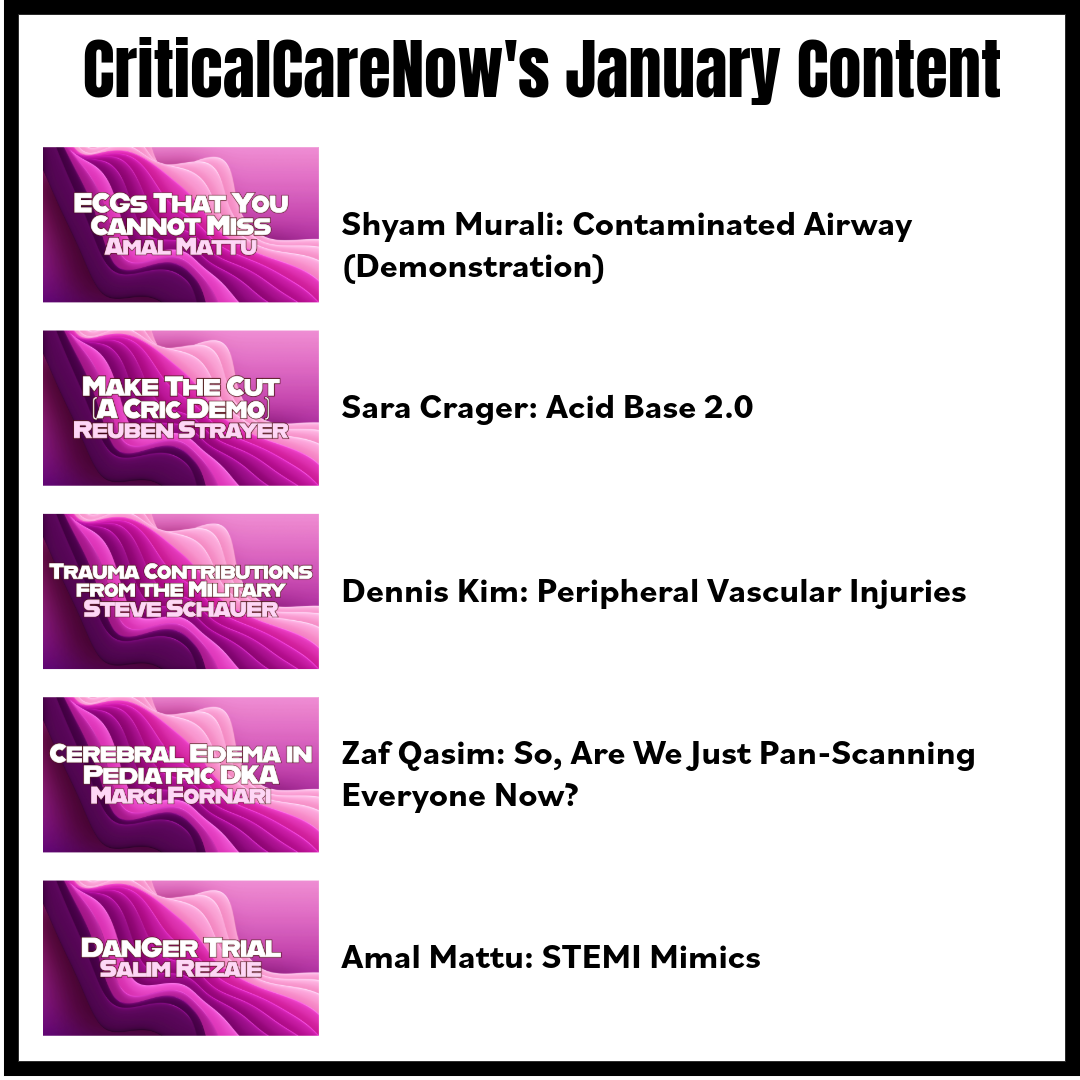
If you're an All-Access Member, you're in for some great content this month. We have FIVE videos hand-picked by our staff that are high-yield and our most highly watched. We're featuring
- Murali on "Contaminated Airway (Demonstration)"
- Crager on "Acid Base 2.0"
- Kim on "Peripheral Vascular Injuries"
- Qasim on "So, Are We Just Pan-Scanning Everyone Now?"
- Mattu on "STEMI Mimics"
Each month we bring you fresh new content from the best of the best in resuscitation. If you're an All-Access member, go watch these videos NOW! If you're not, then sign up here.





Responses