ResusNation #142

A Message From Haney

ResusX 2026 is Coming!
Save the Date: May 18-20, 2026
I'm thrilled to announce that ResusX 2026, the premier resuscitation conference of the year, is returning for its eighth amazing year!
Join us May 18 – 20, 2026, as we return to Philadelphia's iconic Punchline Comedy Club for our most ambitious event yet.
The overwhelming interest we've received through emails and messages has shown just how excited you, the ResusNation, are for this announcement. We're pulling out all the stops to bring you an unforgettable experience featuring the leading voices in resuscitation—live and in person.
Keep reading, because now is your chance to get early-bird tickets. Don't miss your chance to be part of this landmark event in the City of Brotherly Love. Stay tuned for more details about our world-class speakers, innovative sessions, and more.

We're finalizing an action-packed schedule, including specialized post-conference workshops. Full CME and CEU details will be available on our website shortly.
Given the intimate venue and unprecedented interest in ResusX 2026, we anticipate tickets will sell out rapidly.
As a valued newsletter subscriber, we want to ensure you have priority access to registration. So here's how to secure your spot:
If you're committed to attending ResusX 2026, simply complete our priority access form below. You'll receive immediate notification when ticket sales open, giving you the first opportunity to register. Based on the overwhelming response we've already received, we expect tickets to be claimed quickly during this priority registration period.
Complete the Priority Access Form
Evidence-Based Medicine (N=1 Pond)
Imagine, if you will, the absolute chaos of being an Internal Medicine resident in 1750. You have no antibiotics, your stethoscope hasn't been invented yet, and your "UpToDate" is just a dusty scroll that says “Have you tried ghosts?” In this golden era of "trust me, bro" science, European physicians decided that the best way to treat asthma, bruising, and general malaise wasn't rest or rudimentary pharmacology, but literally boiling Kermit the Frog. The logic was surprisingly vibes-based: frogs are slimy and cold; therefore, they must cool down "hot" inflammation. It’s the kind of pathophysiology that would get you kicked out of morning report today, but back then, it was the standard of care.
So, if a patient came in wheezing with an exacerbation, you didn’t reach for a nebulizer or steroids. You reached for a ladle. "Frog Soup" (and its edgy cousin, "Viper Soup") was prescribed with the same straight-faced confidence we currently use for Statins. It was essentially the 18th-century version of a wellness shot, except instead of ginger and turmeric, it was reptile dysfunction and amphibian puree. While we now know that eating a swamp creature doesn't actually stabilize mast cells, you have to respect the hustle of trying to fix asthma with nothing but a cauldron and some misplaced optimism.
Welcome to the 142nd edition of ResusNation!
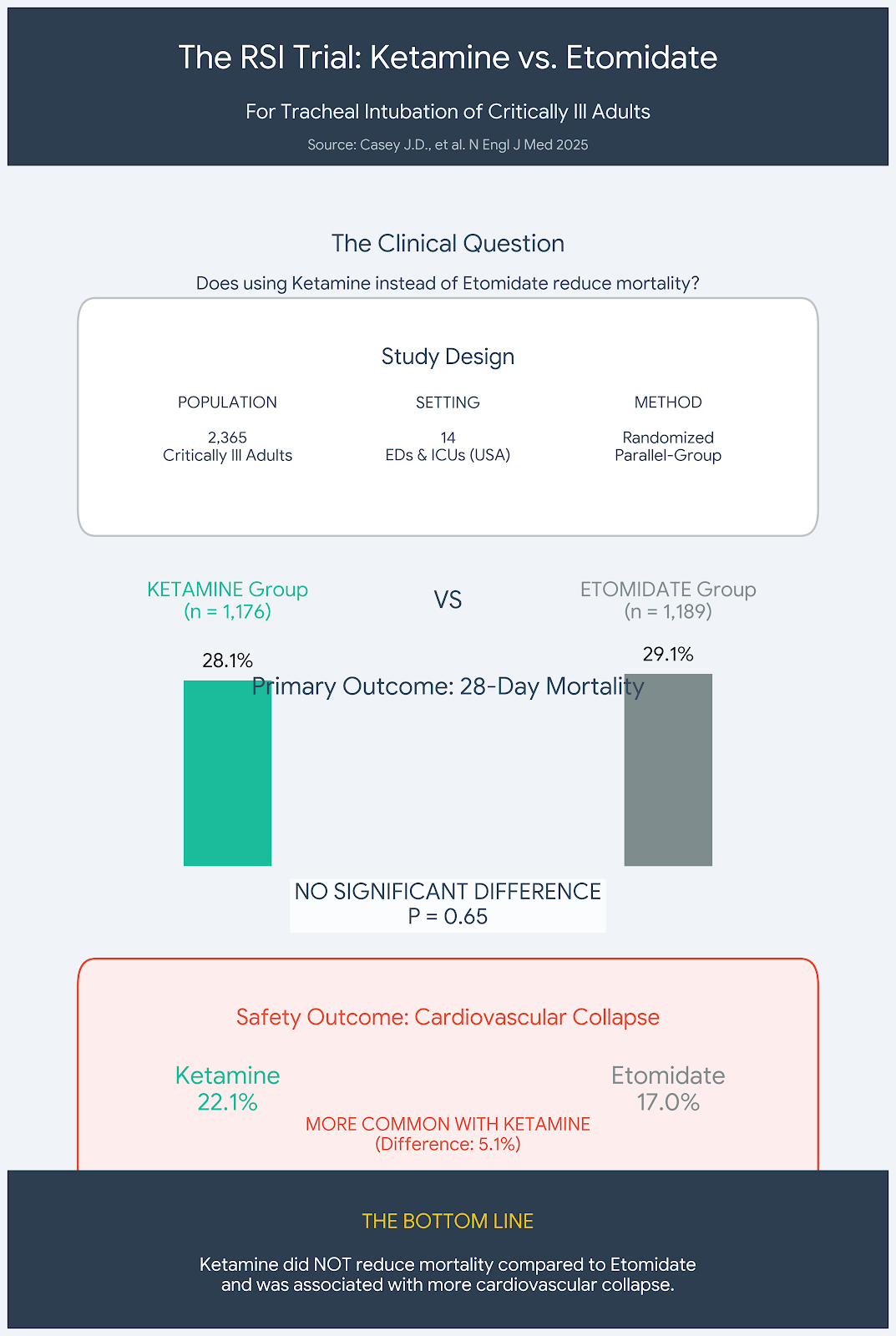
New Data: Is Ketamine Actually Dangerous?
For years, the debate between Etomidate and Ketamine for Rapid Sequence Intubation (RSI) has been as divisive as the "gif vs. jif" argument. I have long leaned on Ketamine for its reputed hemodynamic stability, specifically for patients in shock, while avoiding Etomidate due to lingering concerns about adrenal insufficiency. However, a massive new randomized trial in the New England Journal of Medicine—involving over 2,300 patients—has completely upended my perspective and challenged the clinical dogma we’ve operated under for decades.
While the study showed no significant difference in 28-day mortality, the secondary outcomes were a rude awakening for those of us on "Team Ketamine." The Ketamine group actually experienced more hypotension, increased vasopressor requirements, and higher rates of ventricular tachycardia—even in the sepsis patients we assumed it would protect. This evidence suggests that Ketamine is not the hemodynamically neutral safety net we thought it was. It might be time to swallow our pride, reconsider Etomidate as the superior agent for critical RSI, and let the other side finally say, "I told you so."
Watch the full video here and leave a comment.
Don't forget to like and follow my IG, TikTok, YT, Facebook or Linkedin accounts.


Is Ketamine Really Safer? New Study Challenges RSI Protocols
Emergency intubation is a high-stakes procedure where every second counts, and doctors have long debated which sedative is safest to use. For years, many clinicians favored ketamine, believing it was the better choice for keeping a patient’s heart rate and blood pressure stable during the process. However, a massive new study is shaking up that assumption. Researchers found that using ketamine instead of the standard drug, etomidate, provided no survival benefit for critically ill adults.
In a trial involving over 2,300 patients, survival rates between the two drugs were nearly identical. Even more surprising to the medical community, the patients who received ketamine actually experienced more cardiovascular issues—such as dangerous drops in blood pressure—than those who received etomidate. While this study didn’t look at trauma patients, the results suggest that for most critically ill adults, the standard treatment of etomidate remains a safe and effective choice. This finding helps doctors cut through the noise and make evidence-based decisions when caring for the sickest patients.
Here's my Takeaways:
- Finding: In-hospital death by day 28 occurred in 28.1% of the ketamine group versus 29.1% of the etomidate group ($P=0.65$), showing no significant survival benefit for ketamine
- Practice Impact: Ketamine should not be assumed to be hemodynamically superior; in fact, it was associated with a higher rate of cardiovascular collapse (22.1% vs. 17.0%) compared to etomidate
- Population: Critically ill adults undergoing emergency tracheal intubation in U.S. emergency departments and intensive care units
- Limitation: The study was unblinded and specifically excluded patients with a primary diagnosis of trauma, so results may not apply to that specific group
"Want to learn more? Read the full study "Ketamine or Etomidate for Tracheal Intubation of Critically Ill Adults" by J.D. Casey et al. in The New England Journal of Medicine."

What’s up, ICU nerds?
Welcome back. Grab a coffee, put on your thinking caps, and let’s round!
Today’s edition is a throwback—I’m feeling a bit sentimental. I’ve picked what I consider one of the most interesting critical care trials of the past two decades.
We’re talking about the VASST trial (Vasopressin in Septic Shock) published in NEJM in 2008.
Why this matters:
-
We agree norepinephrine is the first-line vasopressor in septic shock.
-
But as norepi doses rise, so do complications.
-
Vasopressin is catecholamine-sparing—but does it actually improve outcomes?
The Study Facts
What: VASST — A multicenter, randomized, double-blind RCT. Who: 778 patients with septic shock across the U.S., Canada, and Australia.
-
Inclusion: Required ≥5 mcg/min of norepinephrine at randomization.
-
Exclusion: Heart failure, traumatic brain injury, and hyponatremia.
The Intervention:
-
Test Group: Add Vasopressin 0.01–0.03 units/min.
-
Control Group: Continue up-titrating norepinephrine alone.
The Question: Does adding vasopressin, rather than just increasing norepinephrine, reduce mortality?
The Results
Primary Outcome (28-day Mortality):
-
Vasopressin group: 35.4%
-
Norepinephrine group: 39.3%
-
p = 0.26
-
Result: Absolute risk difference around 4% favoring vasopressin, but it did not reach statistical significance.
The "Attention-Grabbing" Sub-group Analysis: In patients with less severe septic shock (norepi 5–14 mcg/min) at randomization:
-
Vasopressin: 26.5% mortality
-
Norepinephrine: 35.7% mortality
-
p = 0.05
TL;DR: VASST showed numerically better survival with vasopressin, but the primary outcome was neutral. However, the signal in less severe shock generated a massive hypothesis.
Does this change my practice?
Honestly? I was already Team Vaso, and this trial only made me dig my heels in further.
Here’s why:
-
Physiology makes sense: We can only saturate so many α-receptors with norepi. Vasopressin works through a different mechanism (V1-mediated vasoconstriction) and helps renal water handling.
-
The signal is there: The study didn’t achieve the huge mortality reduction it was powered for, but the numerical benefit—especially in less severe shock—is hard to ignore.
Was the study underpowered? Was the vasopressin dose too low? Maybe. Either way, the trend matters.
Important Safety Considerations
If you are using Vasopressin, remember:
-
Must use a central line: Do not give peripherally (there is no antidote for extravasation).
-
Higher risk of digital ischemia.
-
Caution in patients with heart failure (remember, they were excluded from VASST for a reason).
What’s next?
The real unanswered question is when to add vasopressin—and at what norepinephrine dose. But that’s a conversation for another day, my friends.
Have you read VASST? Are you Team Early Vaso or Team Norepi Maximalist?
Let me know—I want ALL your vaso-related thoughts.
Until next time, ICUBOY
@icuboy_meded (IG/TikTok/X/Threads) @icuboymeded (FB)
Watch the December's
Videos Now!
If you're an All-Access Member, you're in for some great content this month. We have FIVE videos hand-picked by our staff that are high-yield and our most highly watched. We're featuring
- Spiegel on "65% of the Time The Bougie Works Every Time"
- Khoujah on "Status Epilepticus"
- Crager on "Should That Patient Be On ECMO?"
- Willis on "This Ain't Your Daddy's DKA"
- Byrne on "The Trauma Airway"
Each month we bring you fresh new content from the best of the best in resuscitation. If you're an All-Access member, go watch these videos NOW! If you're not, then sign up here.





Responses