ResusNation #145

A Message From Haney
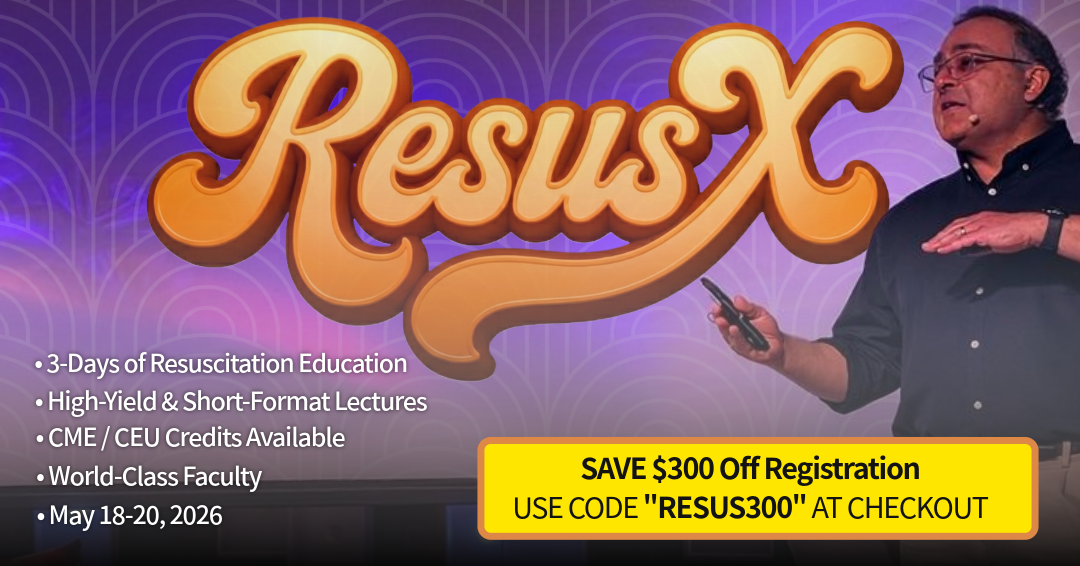
Get ready for ResusX:2026
Three action-packed days of hands-on resuscitation training, real-world simulations, and life-saving strategies! And here’s the best part: we’re giving $300 off your ticket! Just use code RESUS300 at checkout.
Why Attend ResusX:2026?
-
Step into high-stakes clinical scenarios and sharpen your decision-making.
-
Learn from world-leading resuscitation experts.
-
Connect with an unmatched community of clinicians passionate about saving lives.
-
Experience immersive live simulations and interactive cases you won’t find anywhere else.
Special Offer for Non-Attending Clinicians
We haven’t forgotten about you! If you’re a non-attending clinician, fill out this form to receive your unique discount code.

Hurry – Promo Ends February 28, 2026!
After that, ticket prices go back to normal. Don’t miss your chance to join the ultimate resuscitation experience and elevate your skills to the next level.

I Am Groot?
The medical world loves a good "zebra," but Artyom Sidorkin’s case was more like finding a literal unicorn in the middle of a Moscow hospital. Before the viral headlines took over, this started as a standard clinical nightmare: a 28-year-old presenting with classic red-flag symptoms—sharp pleuritic pain and significant hemoptysis. When the imaging came back showing a consolidated mass in the lung, the diagnostic pathway seemed tragically short. In a patient this young, you’re already running through the heavy hitters: aggressive malignancy or a particularly nasty fungal infection. The surgeons went in with a "find and staged" mindset, fully prepared to resect a tumor that was ruining a young man’s life. Instead, they hit a biological plot twist that felt less like surgery and more like a hike in the Ural Mountains.
The surgical team, led by a very confused Dr. Vladimir Kamashev, discovered that the "mass" wasn't a collection of rogue cells, but a 5cm fir branch lodged deep in the tissue. This immediately sparked a scientific debate that pitted "cool internet stories" against the laws of photosynthesis. While the world wanted to believe a seed had magically sprouted in the dark, damp cave of a bronchus, the botany just didn't math out. A germinating seed without sunlight produces a "ghost plant" (etiolated) because it lacks the energy to make chlorophyll. The more likely—and arguably more terrifying—reality is that Sidorkin inhaled a prickly, waxy branch whole. Because of its hardy coating, the branch became a permanent resident, triggering a massive granulomatous reaction that tricked every modern diagnostic tool into thinking it was a terminal illness. It’s the ultimate reminder that while the body is a temple, sometimes it’s also a very efficient, very painful compost bin.
Welcome to the 145th edition of ResusNation!
The NODES Mnemonic
It’s a classic ED scenario: a patient comes in encephalopathic, you push D50, their mental status clears, and you feel like a hero. But here’s the hard truth I’ve learned after countless shifts—if you stop there, you might be failing the patient. The easy part is fixing the number; the real medicine happens when you investigate why they crashed in the first place. Too often, I see clinicians blame missed meals or medication errors and move on, missing the critical underlying pathology hiding in plain sight.
When the cause isn't obvious, I rely on the NODES mnemonic to ensure I never miss a lethal diagnosis. We need to look beyond insulin and sulfonylureas to consider Neoplastic causes like insulinomas, Organ dysfunction (specifically liver and kidney failure), and Endocrine crashes like adrenal insufficiency. Most importantly, we can never forget Sepsis. When I see unexplained hypoglycemia in a septic patient, I know it portends a poor prognosis driven by a hypermetabolic state. Don't just treat the glucose; treat the patient by hunting down the root cause.
Watch the full video here and leave a comment.
Don't forget to like and follow my IG, TikTok, YT, Facebook or Linkedin accounts.


Does Routine Anticoagulant Therapy Help Septic Patients?
Sepsis is one of the most dangerous conditions treated in hospitals, often triggering a chaotic mix of inflammation and blood clotting that can lead to organ failure and death. Because clotting is such a central part of the problem, doctors have long debated whether using "blood thinners" (anticoagulants) could stop this cycle and save lives. However, a major new systematic review involving nearly 7,500 patients is casting doubt on this strategy. After analyzing data from ten different studies, researchers found that giving anticoagulants to a general group of adult sepsis patients did not significantly lower the death rate compared to standard care.
Beyond simply showing no survival benefit, the study highlights a serious caution: patients treated with these drugs showed a trend toward a higher risk of major bleeding. These findings suggest that the routine, "one-size-fits-all" use of blood thinners for every sepsis patient is not effective and could be harmful. While the door isn't closed on using specific treatments like heparin for patients with very specific, severe clotting conditions, this research signals that doctors should prioritize a more personalized approach rather than applying these powerful drugs to everyone.
Here's my Takeaways:
- Anticoagulant therapy provided no significant reduction in all-cause mortality (Relative Risk 0.92) compared to standard care across 7,480 patients.
- The routine administration of anticoagulants to unselected adult sepsis patients is not supported by evidence and should be avoided in clinical practice.
- Adult patients (≥18 years) diagnosed with sepsis, severe sepsis, or septic shock treated in intensive care units.
- A clinically relevant trend toward increased major bleeding events (Relative Risk 1.29) was observed, presenting a potential safety risk.
Want to learn more? Read the full study "Efficacy and safety of anticoagulant therapy in sepsis: A systematic review and meta-analysis" by Jun Lu et al. in the Journal of International Medical Research.
Intubating patients with severe metabolic acidosis—such as those with DKA, lactic acidosis, or renal failure—presents a high risk for sudden cardiovascular collapse. These patients rely on extreme compensatory hyperventilation to maintain a viable pH; however, the transition to mechanical ventilation often causes an inadvertent drop in minute ventilation. This leads to rapid $CO_2$ retention, a "pH cliff," and subsequent hemodynamic failure. The author emphasizes that clinicians must explicitly match or exceed the patient’s pre-intubation minute ventilation during the peri-intubation period to preserve this life-saving respiratory compensation.
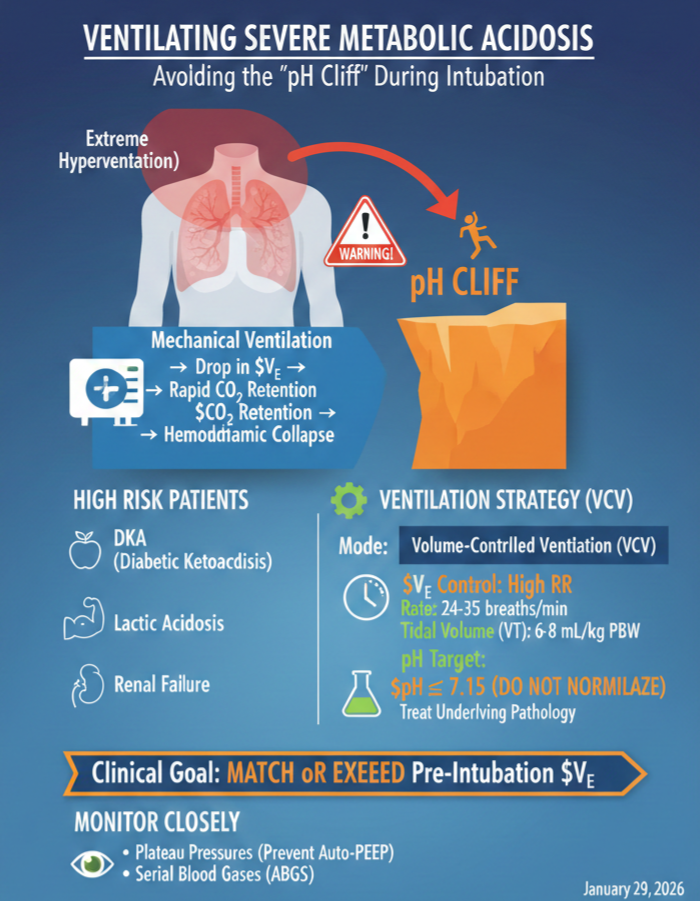
To manage these patients safely, the post recommends using Volume-Controlled Ventilation (VCV) for its predictability and control over $PaCO_2$. The primary strategy involves using a high respiratory rate (often 24–35 breaths/min) as the main lever for compensation, while keeping tidal volumes at 6–8 mL/kg of predicted body weight to avoid lung injury. The goal should not be to normalize the pH, but rather to maintain a target $pH \geq 7.15$ while treating the underlying pathology. Close monitoring of plateau pressures and serial blood gases is essential to prevent auto-PEEP and ensure the ventilator is effectively replacing the patient's work of breathing.
Please read my full post here
Watch the January's
Videos Now!
If you're an All-Access Member, you're in for some great content this month. We have FIVE videos hand-picked by our staff that are high-yield and our most highly watched. We're featuring
- Murali on "Contaminated Airway (Demonstration)"
- Crager on "Acid Base 2.0"
- Kim on "Peripheral Vascular Injuries"
- Qasim on "So, Are We Just Pan-Scanning Everyone Now?"
- Mattu on "STEMI Mimics"
Each month we bring you fresh new content from the best of the best in resuscitation. If you're an All-Access member, go watch these videos NOW! If you're not, then sign up here.






Responses