ResusNation #147

Welcome to ResusNation #147

The Man Who Invented Corn Flakes to Kill Your Libido
If you think modern wellness influencers are unhinged for drinking charcoal lattes, you clearly haven't met Dr. John Harvey Kellogg, the 19th-century king of "clean living" who turned Battle Creek into a high-stakes clinical thirst trap. Kellogg’s medical philosophy was built on the terrifying premise that literally anything fun—flavorful food, caffeine, or any form of "self-love"—was a direct ticket to physical and moral decay. To save the wealthy elite from their own biology, he created a sanitarium that was essentially a luxury spa crossed with a military stockade. Guests paid top dollar to be subjected to a relentless schedule of "biological living," which included being blasted with high-pressure cold water, sitting in electric light baths until they felt like human rotisserie chickens, being repeatedly slapped in the abdomen to aid in digestion, and consuming a diet so bland it was clinically designed to prevent arousal.
The real "main character" of the Kellogg experience, however, was his obsession with the colon. Kellogg believed the gut was a den of iniquity that needed constant, aggressive intervention. We’re talking about a man who championed the "yogurt enema," a procedure that is exactly what it sounds like, followed by the consumption of a pint of yogurt to "re-seed" the flora—basically the OG probiotic, but applied with zero chill. He even invented the corn flake as a weapon against "the vice" of masturbation, believing that bland carbs were the only thing standing between Victorian youth and total societal collapse. It’s the ultimate historical irony: the man who spent his life trying to purge the world of "sinful" impulses ended up giving us the mascot for sugary breakfasts and the foundation for every "gut health" TikTok trend you see today.
Virtual ResusX:2026 Goes LIVE This Monday! (Save 50%)
The wait is over.
On Monday, February 16th you can grab your virtual ticket to ResusX:2026 — and join us from anywhere in the world.
Whether you can’t travel or simply prefer to learn from home, this is your opportunity to experience the energy, insight, and high-yield education that makes ResusX unforgettable.
With your Virtual Ticket, you’ll get:
-
🎥 Access to powerful, high-impact resuscitation talks
-
🧠 Practical clinical pearls you can apply immediately
-
🌎 Earn CME / CEU from the comfort of your own home
-
🔥 The same bold, engaging ResusX experience — streamed to you

ResusX isn’t passive learning.
ResusX is immersive. Practical. Real-world resuscitation education.
Check your inbox on Monday for your 50% discount...these coupon codes will go quick so don't wait!
I can’t wait to have you join us for ResusX:2026.
Haney (@CriticalCareNow)
Your Stethoscope is Obsolete
Look, I’m going to say something that might ruffle some feathers, but we need to be honest with ourselves in 2026. I don't care if you’ve seen thousands of patients or have decades of clinical intuition; if you aren’t integrating bedside echo and ultrasound into your daily practice, you aren’t providing the highest standard of care. We can no longer rely solely on physical exams to guess a patient’s hemodynamic status or fluid responsiveness. Without that visual confirmation, we are essentially flying blind, potentially missing reversible causes or performing procedures with an unnecessary margin of risk that our patients don't deserve.
I’m not saying you need to be a master sonographer or a radiology-level expert overnight. However, you do need to make this a hardwired part of your diagnostic algorithm. Think of POCUS as the new stethoscope—an essential tool that bridges the gap between a "hunch" and a "fact." If you haven't started yet, find a course, shadow a sonographer, or lean on your colleagues. The learning curve is real, but the cost of staying in the dark is far higher. If we want to move the needle on patient outcomes this year, the probe has to become as common as the reflex hammer.
Watch the full video here and leave a comment.
Don't forget to like and follow my IG, TikTok, YT, Facebook or Linkedin accounts.

|
Why "Real Airway Experts" Use Video Laryngoscopy
In this video from ResusX:2025, Dr. Reuben Strayer provides a breakdown of modern airway management, focusing on utilizing video laryngoscopy to our advantage. He argues that the debate between direct and video laryngoscopy is over—but the real question is: which video blade should you reach for first? Dr. Strayer explains why standard geometry video laryngoscopy (SGVL) is the ultimate tool for training and skill retention, and provides techniques to master the "difficult" hyperangulated blade. He also discusses awake intubation vs RSI, and when to pivot to more advanced techniques, such as Video Assisted Flexible Endoscopic Intubation (VAFEI).
Key topics in this video:
- The Brutal History: From Blind Nasal to Paralytics
- The Laryngoscope Evolution (1943 to Today)
- Why the Glidescope Confused Everything
- Standard vs. Hyper-Angulated Blades: The Real Difference
- Why Traditional DL is "Bravado" and Dangerous in Training
- The Tube Delivery Trap: Hyper-Angulated Limitations
- Why Standard Geometry VL is the Best Training Tool
- The 2025 Airway Strategy: Plan A, B, and C
- VAFEI: The Ultimate Difficult Airway Hack
Check out this video of Dr. Reuben Strayer from ResusX:2025 now!


One Size Doesn't Fit All In ARDS
When a patient develops Acute Respiratory Distress Syndrome (ARDS), their lungs aren't just under attack—their entire immune system may be spiraling out of control. This phenomenon, known as a "cytokine storm," occurs when the body releases an overwhelming flood of signaling proteins that were meant to help but end up causing widespread damage. This review explains why ARDS is so life-threatening; the inflammation doesn't stay in the lungs, it travels through the blood, potentially damaging the heart, kidneys, and brain. Patients typically fall into different "subphenotypes" based on how intense this storm is, meaning that two people with the same diagnosis might actually need very different treatments to survive.
Understanding these different inflammatory profiles allows clinicians to move away from "one-size-fits-all" care and toward precision medicine. For instance, patients with the most severe "hyperinflammatory" profile often have much higher risks of death and organ failure, but they may also respond better to specific treatments like steroids or extracorporeal blood purification. While some of these high-tech therapies—like using "nanosponges" to soak up excess toxins—are still in the early testing phase, the evidence is clear: by matching the right treatment to the right immune profile, we can better protect patients from the devastating effects of the cytokine storm. This approach marks a shift from simply supporting the lungs to actively healing the body’s immune response, offering new hope for recovery in even the most severe cases.
Here's my Takeaways:
- ARDS is characterized by a "cytokine storm" where an uncontrolled release of pro-inflammatory mediators, such as IL-6 and TNF−α disrupts the alveolar-capillary barrier and leads to multiorgan dysfunction syndrome (MODS)
- Clinicians should move toward a precision medicine approach by using biomarker-guided strategies to identify specific subphenotypes, which helps in selecting targeted therapies like IL-1 or IL-6 inhibitors and corticosteroids
- While ARDS affects patients with direct lung insults (pneumonia) or indirect triggers (sepsis), the hyperinflammatory subphenotype—common in COVID-19—is associated with significantly higher mortality and fewer ventilator-free days.
Want to learn more? Read the full study "Cytokine storm in acute respiratory distress syndrome" by Merola et al. in the Journal of Intensive Medicine.
Modern Approach to Shock: Recognize, Act, and Save Lives
This week Dr. Jain discusses a modern approach to shock in acute care, emphasizing that we must move beyond the antiquated "one-size-fits-all" mentality of aggressive fluid resuscitation. Instead, he advocates for a physiologically guided strategy that prioritizes the early use of POCUS and dynamic assessments to accurately categorize the type of shock—whether it be distributive, cardiogenic, hypovolemic, or obstructive. Dr. Jain defines shock as a fundamental failure of oxygen delivery to the tissues, and his goal is to teach clinicians how to use real-time tools to determine which patients are truly fluid-responsive, thereby preventing the significant harms associated with fluid overload and venous congestion.
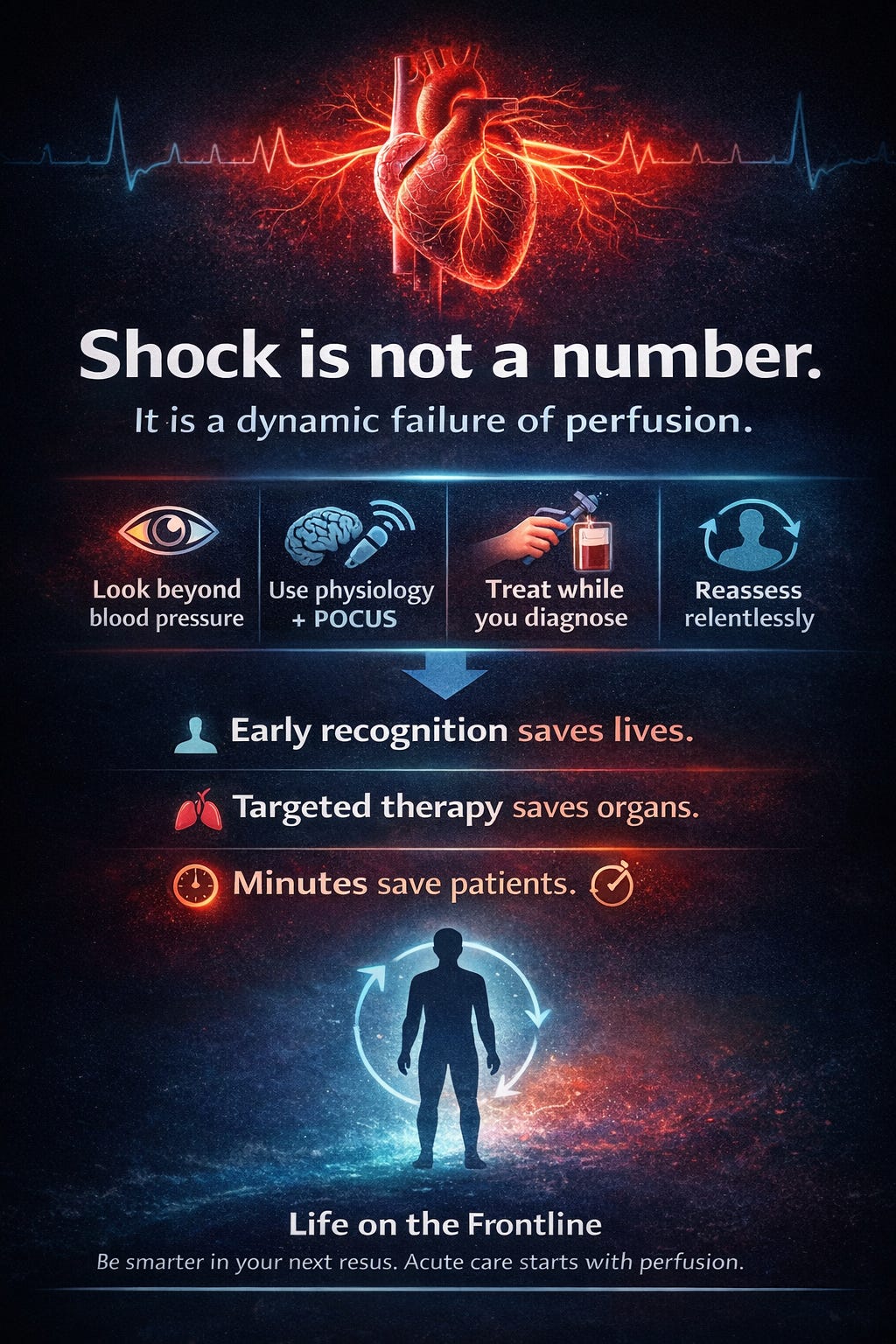
He provides a structured framework for resuscitation that balances the need for immediate hemodynamic support with the necessity of long-term organ protection, and argues that we should be more comfortable initiating vasopressors early to maintain perfusion, rather than waiting for liters of crystalloid to fail. Throughout the article, Dr. Jain breaks down the management of shock into distinct phases—Stabilize, Exclude immediate dangers, and Disposition and definitive care (SED approach)—to ensure that our interventions are as precise as possible. By focusing on metabolic markers like lactate clearance and individualized patient targets, he aims to provide a roadmap for more sophisticated, data-driven care at the bedside.
Read the full post here.
Dr. Arihant Jain is an Emergency Medicine physician at All India Institute of Medical Sciences (AIIMS) in New Delhi, and the creator of Life on the Frontline, a blog sharing concise, evidence-based insights from the ED. He currently serves as a Decision Editor for CPC-EM, is among the youngest ATLS faculty in India, and an AHA-certified BLS/ALCS instructor.
Connect with Dr. Jain:
@humans.of.em (IG)
Watch the February Videos Now!
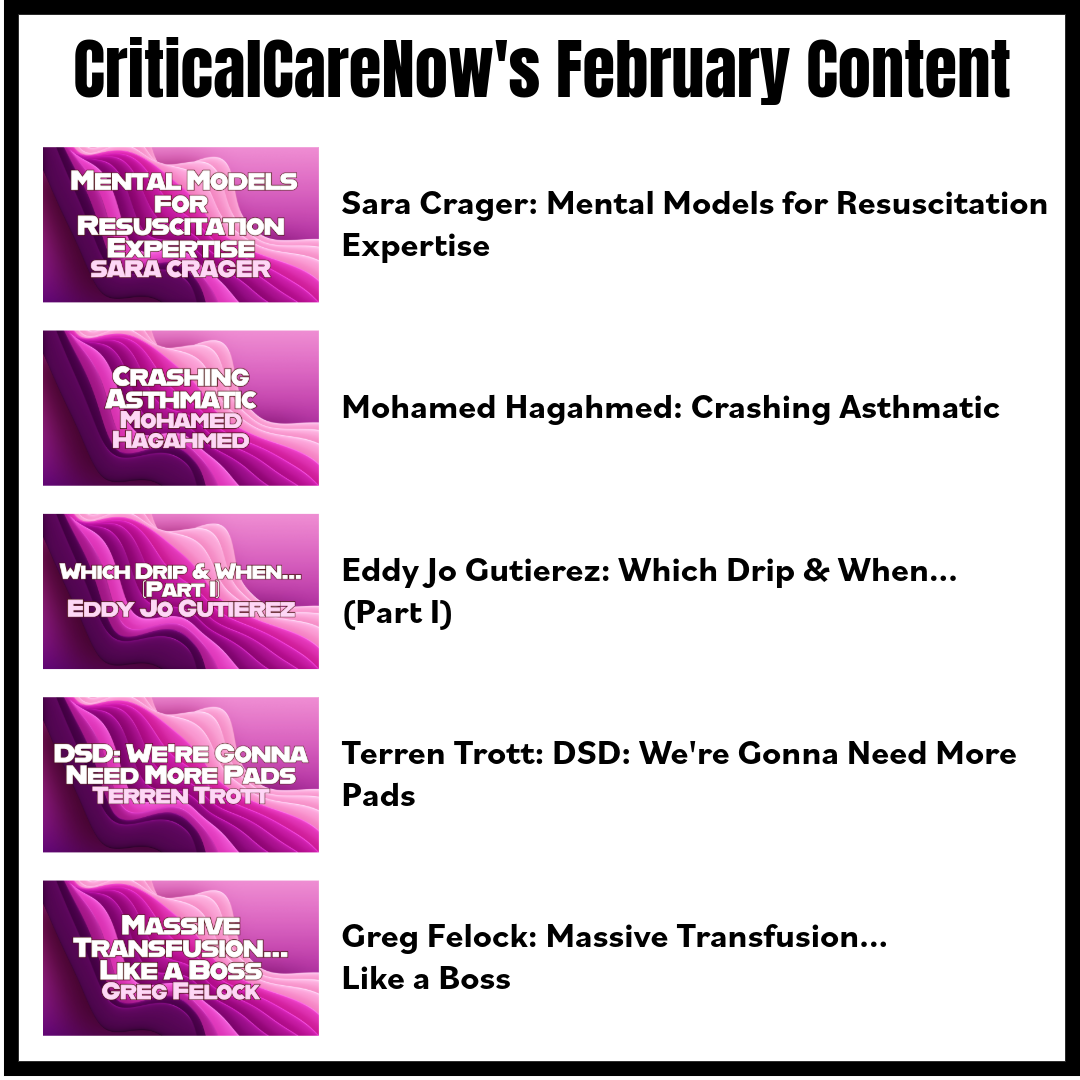
If you're an All-Access Member, you're in for some great content this month. We have FIVE videos hand-picked by our staff that are high-yield and our most highly watched. We're featuring
- Crager on "Mental Models for Resuscitation Expertise"
- Hagahmed on "Crashing Asthmatic"
- Gutierez on "Which Drip & When... (Part I)"
- Trott on "DSD: We're Gonna Need More Pads"
- Felock on "Massive Transfusion... Like a Boss"
Each month we bring you fresh new content from the best of the best in resuscitation. If you're an All-Access member, go watch these videos NOW! If you're not, then sign up here.






Responses