ResusNation #144

A Message From Haney
Welcome to ResusNation #144

Is Your Cat Gaslighting You?
Let’s talk about Toxoplasma gondii, a protozoan with a reproduction strategy so toxic it makes your worst ex look emotionally stable. Toxo has a strict "cats only" policy for sexual reproduction, but it frequently finds itself stuck in intermediate hosts—specifically, rats. In a stunning display of evolutionary 4D chess, the parasite doesn't just wait for the rat to get eaten; it actively facilitates the meal. It hijacks the murine amygdala, effectively deleting the innate fear of predator odors. But it doesn't stop at fear extinction; it flips the valence entirely, creating a specific attraction to cat urine. It’s called "Fatal Feline Attraction," turning the rat into a biological Uber Eats delivery for the cat, just so the parasite can complete its life cycle.
Here is where it gets existentially horrifying for us: humans are accidental hosts, and about one-third of the global population is currently walking around with Toxo cysts camping out in their neural tissue. While we aren't exactly throwing ourselves at mountain lions (usually), the "manipulation hypothesis" suggests Toxo is still pulling strings in the background. Studies have linked latent infection with subtle behavioral shifts toward higher risk-taking—think aggressive driving, entrepreneurship, or thinking you can survive residency on four hours of sleep. Essentially, that impulsive urge to do something stupid might not be "free will"; it might just be a microscopic organism trying to get you eaten by a predator that hasn't hunted us in 10,000 years.
Welcome to the 144th edition of ResusNation!
Why I’m Choosing This Over Propofol More
I was lucky enough to be on the Board Bombs podcast and we talked about how I used to treat Precedex (Dexmedetomidine) as a luxury item—great in theory, but often too expensive to justify. Now that it’s off-patent and widely available, it has become an indispensable tool in my practice, primarily because it solves the biggest headache with sedation: respiratory depression. Unlike Propofol or heavy benzodiazepines, I can use Dex to sedate an anxious, non-intubated patient without the constant anxiety that I’m about to wipe out their respiratory drive. It gives us that "sweet spot" of a calm patient who is still protecting their own airway.
But where this drug really shines is in its versatility beyond simple sedation. It acts on spinal pain receptors to actually potentiate opioids, making it a game-changer for managing pain in opioid-tolerant patients without reaching dangerous dosage ceilings. Furthermore, for those of us working in urban EDs, its sympatholytic properties make it incredible for mitigating withdrawal symptoms—breaking the cycle of tachycardia and hypertension just like clonidine. It’s not just a sedative; it’s a multi-modal safety net that too many of us are underutilizing.
Watch the full video here and leave a comment.
Don't forget to like and follow my IG, TikTok, YT, Facebook or Linkedin accounts.

Reducing Hypoxemia Risks During RSI
For critically ill patients, the moments before a breathing tube is inserted—known as intubation—are some of the most dangerous in their hospital stay. If a patient’s oxygen levels drop too low during this procedure (a condition called hypoxemia), it can lead to severe complications like cardiac arrest or even death. To prevent this, doctors "preoxygenate" patients, essentially filling their lungs with an oxygen reserve before the procedure begins. A recent systematic review has found that using noninvasive ventilation (a tight-fitting mask connected to a ventilator) is significantly better at maintaining safe oxygen levels than the traditional method of manually squeezing a bag-valve-mask.
The study suggests that noninvasive ventilation (NIV) pushes oxygen into the lungs more effectively, keeping airways open better than the manual bag method. While the research showed that NIV clearly reduces the risk of dangerous oxygen drops, it is important to note that it didn't change overall survival rates or the risk of vomiting (regurgitation) during the procedure. Despite this, preventing hypoxemia is a critical win for patient safety. These findings suggest that hospitals should consider making NIV the standard "go-to" for preoxygenating high-risk patients, potentially updating clinical guidelines to ensure the safest possible care during emergencies.
Here's my Takeaways:
- Noninvasive ventilation significantly reduced the risk of hypoxemia during intubation compared to bag-valve-mask ventilation, showing a 93% probability of benefit.
- Clinicians should integrate noninvasive ventilation as a standard practice for preoxygenation in high-risk patients to prevent dangerous oxygen drops.
- Critically ill adult patients with acute respiratory failure undergoing emergency tracheal intubation.
- The study found no significant difference in all-cause mortality or regurgitation rates, suggesting the benefit is primarily limited to oxygen saturation levels rather than broader survival outcomes.
Want to learn more? Read the full study "Effectiveness of noninvasive ventilation for preoxygenation in emergency intubation: a systematic review and meta-analysis" by Gioli-Pereira et al. in Critical Care Science.
Get ready for ResusX:2026
Three action-packed days of hands-on resuscitation training, real-world simulations, and life-saving strategies! And here’s the best part: we’re giving $300 off your ticket! Just use code RESUS300 at checkout.
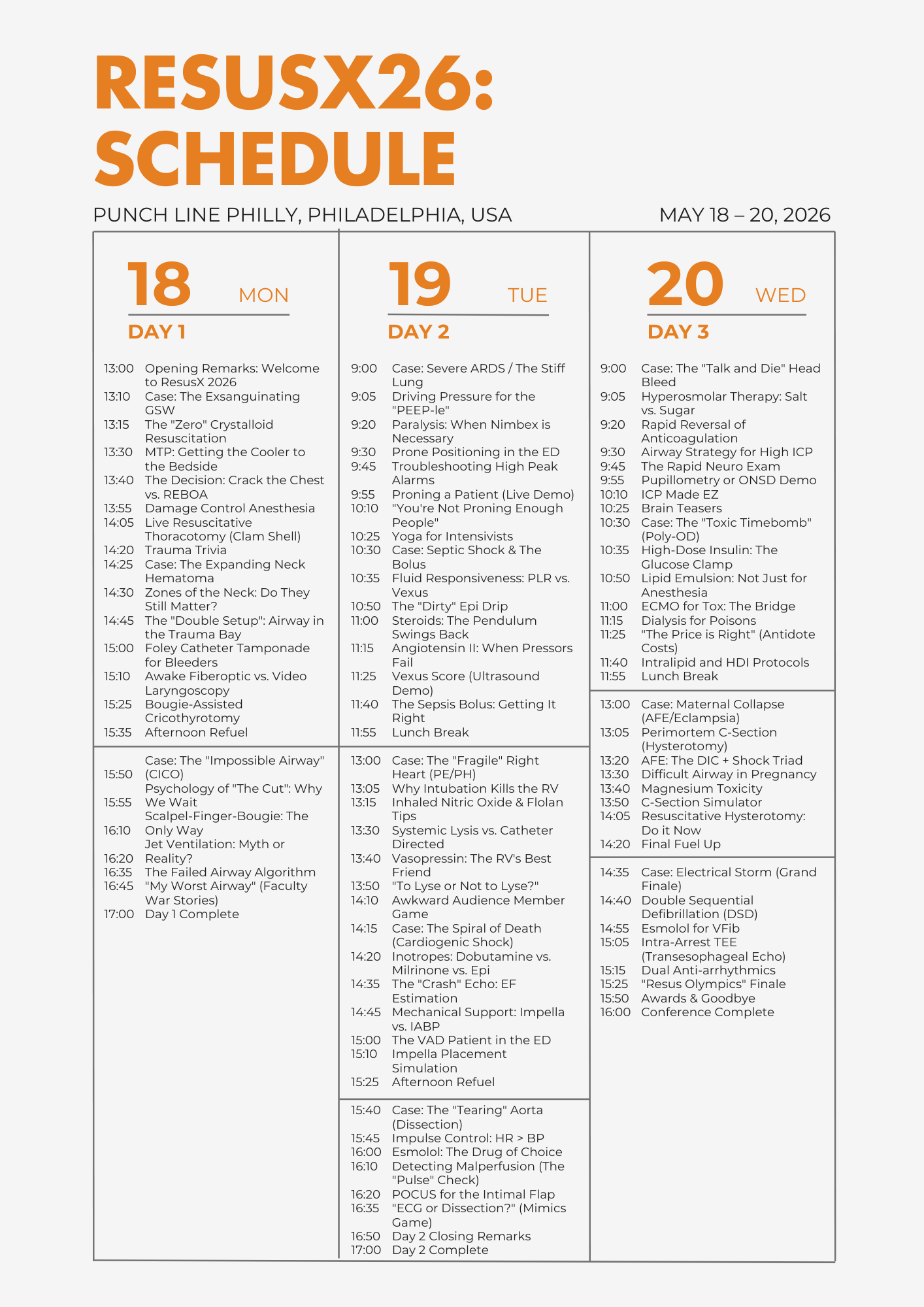
Why Attend ResusX:2026?
-
Step into high-stakes clinical scenarios and sharpen your decision-making.
-
Learn from world-leading resuscitation experts.
-
Connect with an unmatched community of clinicians passionate about saving lives.
-
Experience immersive live simulations and interactive cases you won’t find anywhere else.
Special Offer for Non-Attending Clinicians
We haven’t forgotten about you! If you’re a non-attending clinician, fill out this form to receive your unique discount code.

Hurry – Promo Ends February 28, 2026!
After that, ticket prices go back to normal. Don’t miss your chance to join the ultimate resuscitation experience and elevate your skills to the next level.

Rounds with ICUBOY
What’s up, ICU Nerds?
I missed you guys.
So lately, I’ve been reading some guidelines (as one does, casually, in their free time). Specifically: the American Heart Association’s Guideline on “Atrial fibrillation occurring during acute hospitalization” aka acute afib.
And I figured – not everyone has time/energy to read through a 22-page guideline/scientific statement. And then I thought – why not include my top take-aways from this guideline in the newsletter. And here we are!
Forewarning: these guidelines were published in 2023, so they’re not exactly a spring chicken. But I still think they’re worth being familiar with.
Some key points I learned:
-
Acute afib is afib detected in an acute care setting or during an acute illness. This might be afib that developed secondary to the illness itself OR it could be afib that existed before the acute illness, but no one had detected yet.
-
Acute afib is INCREASING in incidence. How common is it?
a. Septic shock: up to 44%
b. Post CABG: 32%
c. Post CABG + aortic valve replacement: 49%
d. Post CABG + mitral valve replacement: 64% -
It’s NOT as benign as we once thought it was. Acute afib is associated with longer hospitalizations, high rates of recurrence, and greater morbidity & mortality.
-
Risk factors for developing acute afib (or “substrates” as they’re labeled in the guidelines) include:
a. Prior cardiac surgeries including prior valvular surgery
b. Atrial scars from chronic pressure overload ie chronic HTN, CKD
c. Prior pulmonary disease -
Triggers that might tip a patient over into acute afib are well known to us including inflammation, electrolyte imbalances, sepsis, bleeding, volume changes, need for inotropes, etc.
-
Some aspects of management are crystal clear, such as:
a. If the patient is HD unstable → direct current cardioversion; start with higher voltage upfront, pads in antero-posterior position
b. Always search for & treat the underlying cause -
Some aspects of management leave me wishing it was a bit more crystal-clear, and less wishy-washy, such as:
a. The age-old question, should I do rate or rhythm control?
i. “Because acute AF may spontaneously convert to sinus, an initial rate control […] wait and see approach may be reasonable for HD stable asymptomatic patients”
ii. Rhythm control poses some challenges including:
1. Risk of acute thromboembolism & stroke
2. Need for sedation with electrical cardioversion
3. Risk of QTc prolongation, especially with amiodarone -
“The prior concept of safe to cardiovert without further assessment or anticoagulation if AF duration has been 48 hours or less has been challenged”
a. Cardioversion 12 hours or more after afib onset is an independent predictor of thrombo-embolic complications!
b. Not surprisingly, the risk increases as the CHADS-VASc score does!
c. Don’t be too gutsy about this…
d. You need a TEE to rule out an intra-cardiac thrombus or 3 weeks of religious compliance with anticoagulation BEFORE cardioversion.
e. Regardless of whether cardioversion is chemical or pharmacological, you need 4 weeks of uninterrupted anticoagulation after cardioversion. -
Some final cool miscellaneous points/thoughts
a. Avoid CCBs in patients with EF 40% or less due to negative inotropy (class 3 recommendation = you are harming patients if you do this!)
b. Rhythm control may be better for younger patients with less comorbids and more recent onset afib and low EF that may be caused by tachy-arrhythmia
c. “Available evidence does NOT favor routine acute anticoagulation in patients with sepsis and acute AF”. At the same time, critically ill-patients with new-onset AF have >2x risk of in hospital ischemic stroke compared with those without AFib. Catch 22, if I ever saw one…
It’s not easy folks! Then again, if it were, where would the fun be in that?
I personally continue to believe afib remains a challenging arrhythmia to treat (correctly) as there are a lot of potential factors to consider. Don’t get me wrong – it’s very easy to treat incorrectly (ie diltiazem-for-all approach or being too shock-friendly and not caring about BP or prior anticoagulation), but we need to remain humble and curious for the wellbeing of our patients.
Anyway - Keep doing your best out there.
See ya next time!
ICUBOY
@icuboy_meded (IG/TikTok/X/Threads)
@icuboymeded (FB)
Watch the January's
Videos Now!
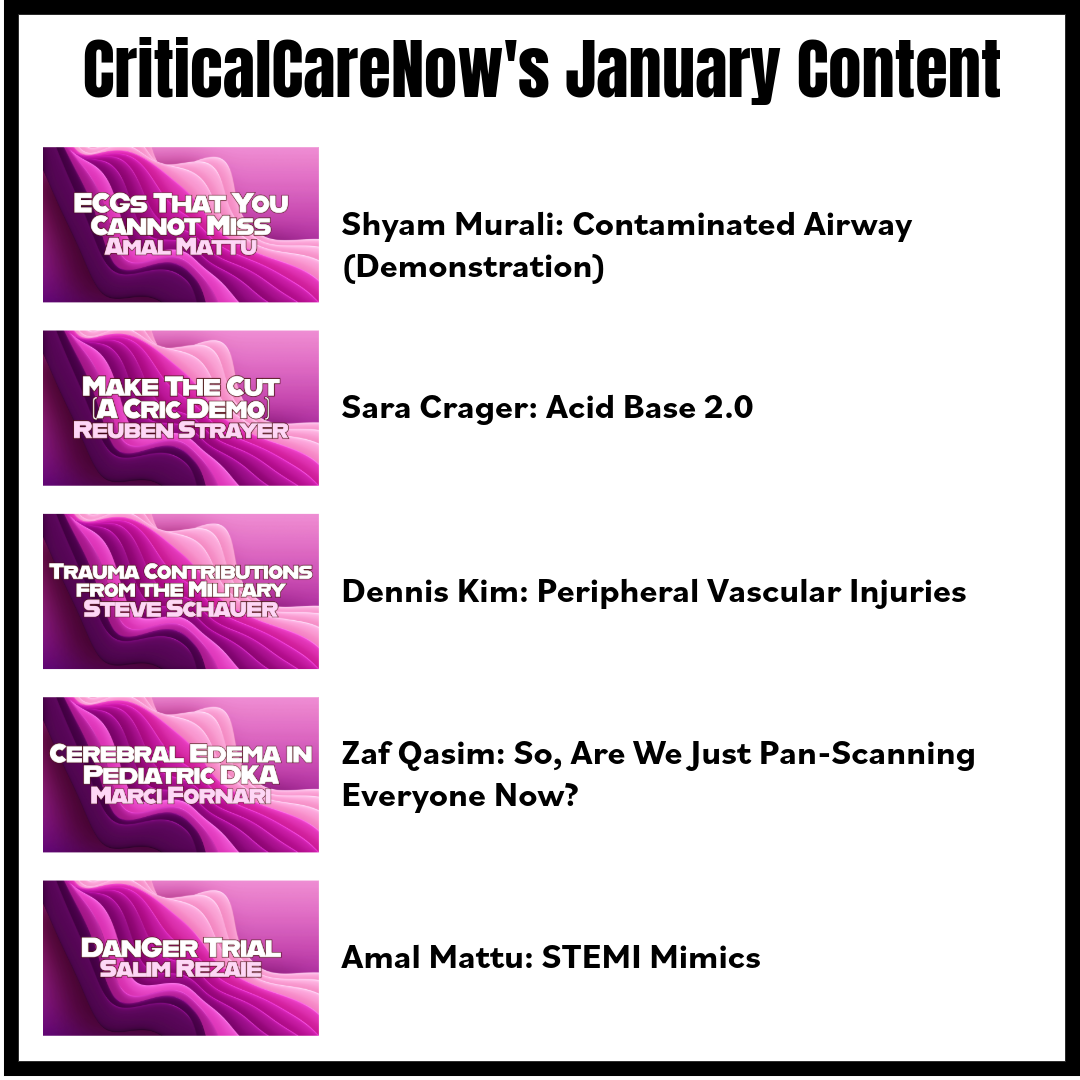
If you're an All-Access Member, you're in for some great content this month. We have FIVE videos hand-picked by our staff that are high-yield and our most highly watched. We're featuring
- Murali on "Contaminated Airway (Demonstration)"
- Crager on "Acid Base 2.0"
- Kim on "Peripheral Vascular Injuries"
- Qasim on "So, Are We Just Pan-Scanning Everyone Now?"
- Mattu on "STEMI Mimics"
Each month we bring you fresh new content from the best of the best in resuscitation. If you're an All-Access member, go watch these videos NOW! If you're not, then sign up here.






Responses